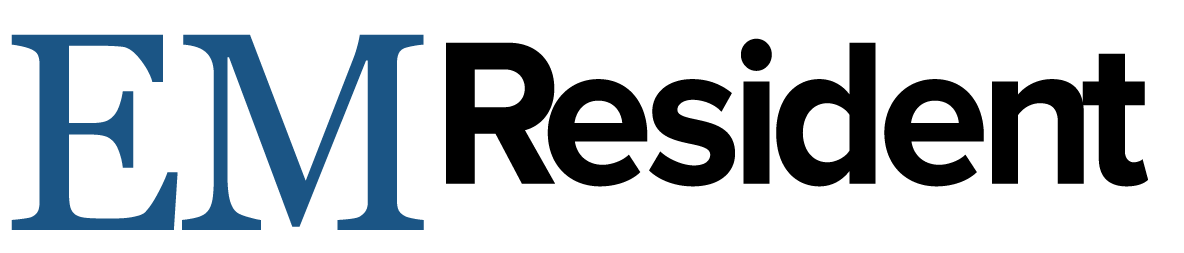
A 54-year-old male with a past medical history significant for primary CNS B-cell lymphoma, on chemotherapy and lacosamide for seizure prophylaxis, was admitted to the ICU for hypoxia and neutropenic fever. What is your interpretation of his ECG?
Answer
This ECG shows atrial fibrillation with a ventricular rate of 110 bpm, normal axis, and coved STE > 2 mm followed by a negative T-wave in leads V1-V2.
The differential diagnosis for STE in lead V1 includes:
- Acute MI (anteroseptal or right ventricular)
- Acute RV strain (eg, PE)
- Brugada syndrome
- Hyperkalemia
- LBBB
- LVH
- Sodium channel blocker toxicity
- Ventricular-paced rhythm
The findings in this ECG are consistent with Brugada ECG pattern. The initial Brugada ECG criteria set forth in 20021 included 3 types:
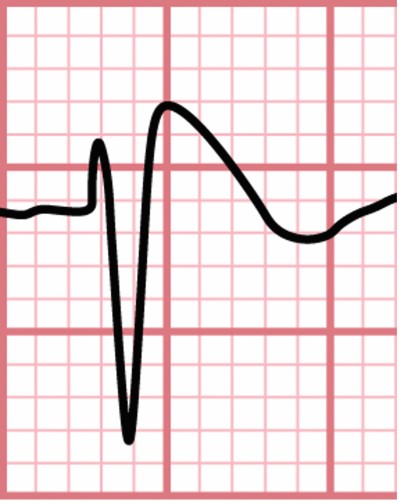
- Type 1: Coved STE ≥ 2 mm followed by a negative T-wave in > 1 of leads V1-V3 (see Figure 1)
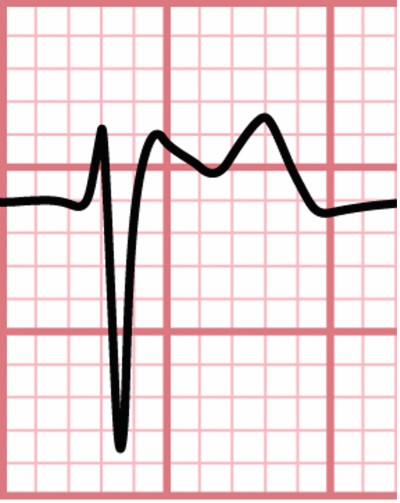
- Type 2: ≥ 2 mm of saddleback shaped STE in > 1 of leads V1-V3 (see Figure 2)
- Type 3: Type 1 or 2 morphology not meeting above criteria in > 1 of leads V1-V3
More recent 2013 guidelines2 narrowed the definition: “Brugada syndrome is diagnosed in patients with ST-segment elevation with type 1 morphology ≥ 2 mm in ≥ 1 lead in the right precordial leads V1, V2, positioned in the 2nd, 3rd, or 4th intercostal space occurring either spontaneously or after provocative drug test with intravenous administration of class I antiarrhythmic drugs.”
The important changes in the new definition include:
- Type 1 is the only potentially diagnostic pattern
- Type 1 only needs to be seen in one lead and can be seen in lead(s) V1/V2 when positioned higher than the traditional 4th intercostal space
- Type 2 is non-diagnostic and it is only clinically significant if the Type I pattern is seen or can be provoked with sodium channel blocking antidysrhythmics
- Type 3 is no longer part of the criteria
- Lead V3 is no longer part of the criteria
Brugada syndrome is caused by a mutation in the cardiac sodium channel gene (ie, a sodium channelopathy) that can lead to unprovoked dysrhythmias (polymorphic ventricular tachycardia or ventricular fibrillation) and cardiac arrest. The diagnostic criteria include both ECG changes and clinical criteria (see Learning Points below). Notably, up to 40% of patients with Brugada syndrome will have normal resting ECGs. Treatment for Brugada Syndrome is placement of an automatic implantable cardioverter-defibrillator for prevention of sudden cardiac death.
The Brugada ECG pattern can be provoked by multiple conditions, including fever and medications, in particular sodium channel blocking medications. In this case, the patient had both a fever and was taking lacosamide (which has sodium channel blocking properties), either or both of which could have contributed to the changes seen on his ECG. The significance of this finding depends on the patient’s clinical history, as the diagnostic criteria for Brugada syndrome include both ECG and clinical criteria.
Case Conclusion
The patient was evaluated by Electrophysiology, who recommended fever control and discontinuing any medications with sodium channel blocking properties. Further diagnostic workup for Brugada syndrome was deferred given the lack of clinical criteria and variable utility and accuracy of electrophysiology studies for asymptomatic patients with fever-induced Brugada.
Brugada Syndrome Learning Points
- Sodium channelopathy that can lead to unprovoked dysrhythmias (polymorphic ventricular tachycardia or ventricular fibrillation) and cardiac arrest
- Diagnosis made from both ECG and clinical criteria (see table)
- Type 1 is the only ECG abnormality that is potentially diagnostic
- Type 2 is non-diagnostic but warrant further investigation in the appropriate clinical situation
- Type 3 is no longer considered useful in diagnosis
- Treatment is AICD placement
|
ECG Criteria |
Clinical Criteria (must have ≥ 1): |
|
§ Complete or incomplete RBBB pattern with coved STE ≥ 2 mm followed by a negative T-wave in ≥ 1 of leads V1-V2
|
§ Documented VF or polymorphic VT § Family history of sudden cardiac death at < 45 years old § Coved-type ECG in family members § Inducibility of VT with programmed electrical stimulation § Syncope § Nocturnal agonal respiration |
References
- Wilde AAM, Antzelevitch C, Borggrefe , et al., for the Study Group on the Molecular Basis of Arrhythmias of the European Society of Cardiology. Proposed Diagnostic Criteria for the Brugada Syndrome Consensus Report. Circulation. 2002;106(19):2514-2519.
- Sieira J, Brugada P. The definition of the Brugada syndrome. Eur Heart J. 2017;38(40):3029–3034.