Sarah H. Michael, DO, MS, Resident, Detroit Receiving Hospital, Detroit, MI
There are few tasks in emergency medicine that are as simple to perform — and also as deeply satisfying — as the draining of an abscess. The procedure requires almost no skill, yet it brings practically instantaneous relief for the patient and similarly rapid gratification to the physician. However, the converse is also true — there is a special kind of disappointment that comes when you stick a knife into a red, hot, indurated, fluctuant... cellulitis.
When compared to abscesses, cellulitis just isn't nearly as rewarding. There's nothing even remotely gratifying there; especially after you've cut a hole in it. Ultrasound is now standard use in most adult EDs around the country. This allows the technology to rapidly and easily differentiate the two, and even to identify small abscesses within areas of cellulitis. Ultrasound has transformed emergency medicine and is a perfect non-invasive tool for improving diagnostic accuracy and procedural planning. Still, some of the smaller nuances of ultrasound for soft tissue infections are lesser known to many practitioners of emergency medicine.
Ultrasound is highly effective for identifying soft tissue planes and abnormalities within them, usually with habitus and user skill as the only major complicating factors. Since frequency and depth of sonographic penetration are inversely proportional, using a high-frequency linear transducer for superficial areas of interest, and a lower frequency curvilinear one for deeper structures generally is best practice. In ultrasound of the soft tissues, the skin, subcutaneous tissue and fat, and fascia should be visible; generally, you can also observe muscle and additional fascial layers, depending on the location.
The epidermis and dermis typically will appear as a single thin hyperechoic stripe superficial to the comparatively hypoechoic subcutaneous tissue and fat. Beneath that, you will often find multiple thin hyperechoic facial planes and dense muscle fascicles. Tendons, if present, usually are also visible and are distinguished by their symmetric and linear fibers. Flexion or extension of the adjacent joint will typically accentuate both tendons and muscle bellies. All of these soft tissues should be in relative approximation to each other without separation by hypoechoic fluid, which is what would be expected in the presence of infection.
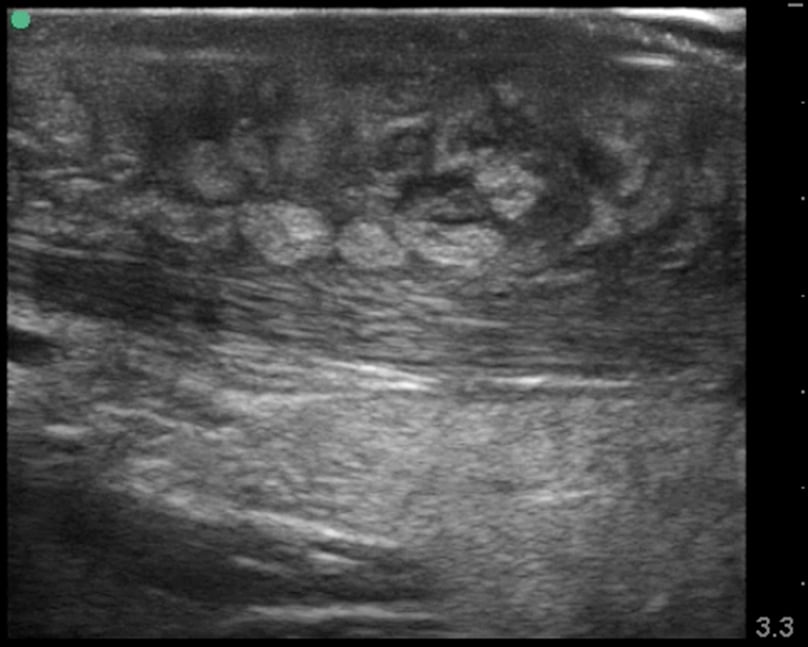
Generally, when you're trying to differentiate an abscess from cellulitis, the infection will be in the subcutaneous tissue, so focus your attention on this area. Deeper infections are possible, and may affect fascia, muscles, or other tissues. Be vigilant, and inspect all of the borders of the infection to help rule out something that may need surgical management. In the case of cellulitis, the ultrasonographic appearance will change as the infection progresses. Early infection may result in swelling and a relatively hyperechoic appearance of the skin and subcutaneous tissue. If you're unsure, consider looking at the unaffected tissues or contralateral side for comparison. As cellulitis evolves, the adipose of the subcutaneous tissues will become infiltrated with hypoechoic fluid, leading to the classic “cobblestone” appearance (Images 1 and 2).
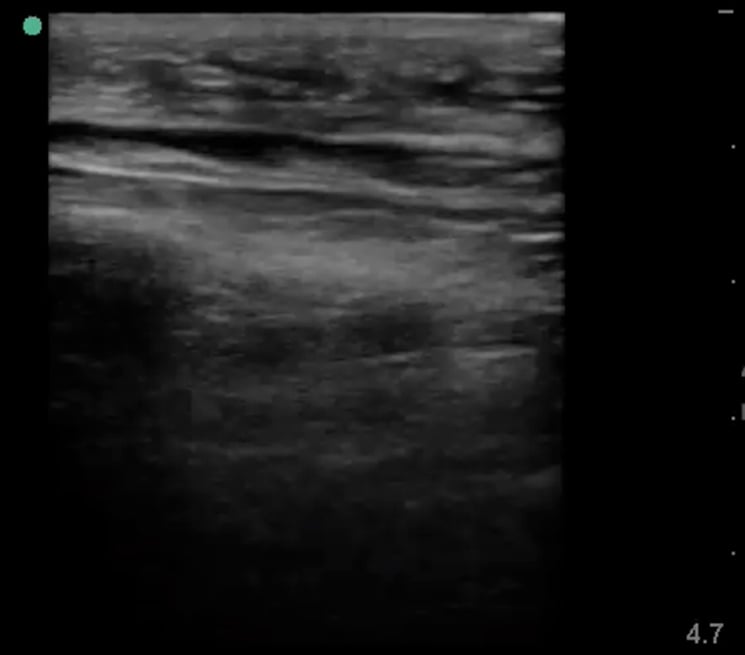
Abscesses may be seen without associated cellulitis, or within it. Evaluate for hypoechoic areas that may or may not be septated. Having an idea of loculations within an abscess can also help you plan your procedural approach. Additionally, while abscess cavities are often seen as uniformly hypoechoic, they can appear to have different echogenicities mixed within them. Abscess material with different densities will appear with varying echogenicity on ultrasound (Image 3). One potential pitfall to be wary of is that an evolving hematoma may also appear as a hypoechoic structure on ultrasound, so clinical history and physical exam findings can be as important as the ultrasound exam.
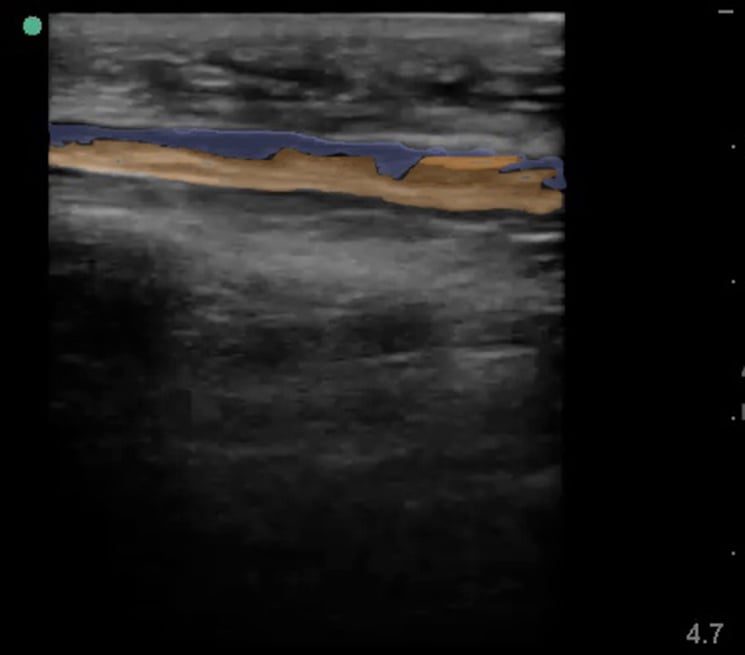
Occasionally ultrasound examination of a fluid collection will reveal vessels nearby or directly underneath the infection. Similar to performing an I&D for peritonsillar abscess, knowledge of presence and depth may alter either the procedure or the clinical decision-making. Depending on the scenario, these fluid collections may actually represent an arterial pseudoaneurysm. Worse than the letdown of incising a cellulitis is the hemorrhage caused by opening an artery. Most ultrasound machines provide a coloring modality that can be used to differentiate vascular structures if there is clinical uncertainty.
At least one study has suggested that ultrasound-guided needle aspiration may be inferior to incision and drainage for management of community-acquired MRSA abscesses,1 though anecdotal evidence is fairly ubiquitous supporting its use. When presented with an abscess, it may be reasonable to first attempt a less invasive ultrasound-guided needle aspiration, and then, if not successful, proceed to incision and drainage. This may be especially advisable in cosmetically important areas like the face.
It is still standard of care to perform complete incision and drainage with a scalpel, despite widely varying practice patterns. If you plan to use needle aspiration, the shortest appropriate large-bore needle that can be found should be used (as appropriate for the given area), followed by sonograpahic re-examination of the previously identified fluid collection. Like other ultrasound-guided procedures, it is best to visualize the needle entering the fluid collection on the screen in real-time.
There is another important learning point to consider — when you're expecting to find either a cellulitis or an abscess on ultrasound, but you find neither, be on the lookout for necrotizing fasciititis. You may see fluid tracking on or between fascial planes and areas of “dirty” shadowing, consistent with gas artifact (Images 4 and 5). As you know, this is a surgical emergency, and the appropriate resources should be quickly mobilized.
By integrating a more advanced knowledge of soft tissue ultrasounds to your decision-making, your procedures will be both more satisfying and successful. By considering potential pitfalls on ultrasound and abscess mimics, you can reduce your complication rate and perhaps save patients from unwarranted invasive procedures.