If you hear hoofbeats it just might be a Zebra...
Grace Bunemann, OMS II - Campbell University School of Osteopathic Medicine
EMRA MSC Osteopathic Coordinator, 2021-2022
People always say that college will bring some pretty amazing people into your life. For me one of those people is Courtney. Courtney is one of my best friends and an all-around incredible person, and she now works as a Pediatric Genetic Counselor for a large university hospital system. But what really makes her special is that she lives with a rare genetic condition called Loeys-Dietz syndrome (LDS) -- a connective tissue disorder. We have all heard “when you hear hoofbeats, think horses, not zebras” from a professor while in medical school but zebras do exist and we can’t afford to miss them!
Loeys-Dietz syndrome was first observed and described by Dr. Bart Loeys and Dr. Hal Dietz at Johns Hopkins University in 2005. Individuals with LDS exhibit a wide variety of medical features in their cardiovascular, musculoskeletal, skin, and gastrointestinal systems. No two people with LDS will have identical medical characteristics as LDS manifests itself in a number of ways. LDS is most often associated with other connective tissue diseases including Marfan syndrome, Vascular Ehlers-Danlos syndrome, and Familial Thoracic Aortic Aneurysm and Dissection.
Many connective tissue disorders have large variation in presenting features like LDS and therefore can go undetected. Undiagnosed patients are unknowingly at increased risk for serious medical complications. The most commonly experienced emergent health crisis in those with connective tissue disorders is aortic dissection. As future emergency medicine physicians, we can help by knowing the signs and symptoms of acute aortic dissections leading to prompt treatment and recommendation of future specialized care.
Specifically, triage staff can play a vital role in ensuring patients receive proper care as the first point of contact in an emergency department. Recognizing potentially life-threatening conditions and quickly moving patients along in the treatment process is imperative to preventing adverse outcomes. Patients with an aortic dissection may not appear as the “typical” chest pain patient. Your suspicion should be raised in a patient who is young, tall, thin, and has no known risk factors for heart disease. Approximately 10,000 people experience aortic dissections annually so as emergency physicians it is very likely we will see patients with this condition. Fifty percent of patients with undiagnosed aortic dissection die within 48 hours. Dissections of the aortic root and ascending aorta require immediate surgical intervention. It is extremely important that emergency department staff can recognize the signs of aortic dissection, including some that are less common, and consider the bigger picture.
Evaluation Pathway:
CONSIDER ACUTE AORTIC DISSECTION IN ALL PATIENTS PRESENTING WITH:
- Chest, back, or abdominal pain
- Syncope
- Symptoms consistent with perfusion deficit (i.e. CNS, mesenteric, myocardial, or limb ischemia)
FOCUSED BEDSIDE PRETEST RISK ASSESSMENT FOR ACUTE AORTIC DISSECTION:
- Marfan syndrome, Loeys-Dietz syndrome, or Vascular Ehlers-Danlos syndrome
- Connective tissue disease
- Family history of aortic disease
- Known aortic valve disease (especially bicuspid aortic valve)
- Recent aortic manipulation
- Known thoracic aortic aneurysm
HIGH-RISK PAIN FEATURES:
- Abrupt in onset or severe in intensity and
- Ripping/tearing/sharp or stabbing quality
HIGH-RISK EXAM FEATURES:
- Evidence of perfusion deficit
- Pulse deficit
- Systolic BP differential
- Focal neurologic deficit (in conjunction with pain)
- Murmur of aortic insufficiency (new or not known to be old and in conjunction with pain
- Hypotension or shock state
Keep in mind that a normal EKG or chest radiograph does not rule in or out the possibility of an aortic dissection. If aortic dissection is even remotely suspected, studies like a contrast CT scan should be performed and read as soon as possible – waiting could be the difference between life and death.
When you hear hoofbeats remember it just might be a zebra!
Related Content


May 02, 2023
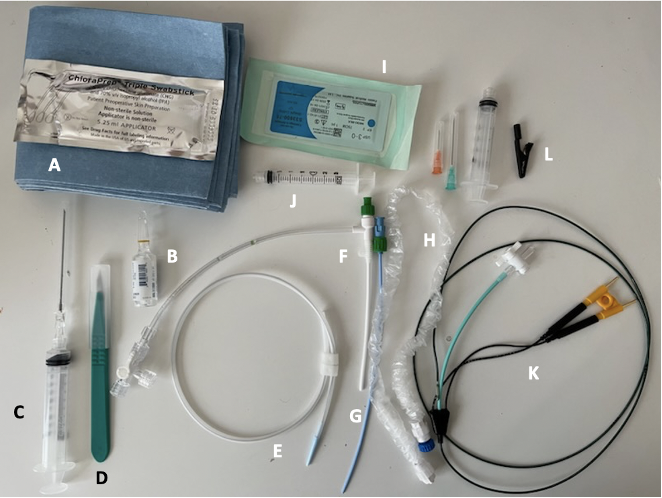
Critical Care Device Series: Transvenous Pacemaker
Temporary transvenous pacing (TTVP) utilizes central venous access to pass an electrode into the right ventricle. TTVPs are one of the most infrequently performed procedures by emergency physicians; however, it is essential for those working in any setting with critically ill patients to be well-equipped to perform this procedure emergently.




