Effects of the COVID-19 Pandemic on International Medical Graduates
Matthew Carvey MD, EMT-P, FP-C
EMRA MSC International Representative, 2021-2022
Tyler Rigdon, MSIV
EMRA MSC West Coast Representative, 2021-2022
The COVID-19 pandemic has led to unprecedented impacts for the medical student community concerning scheduling of rotations, application timelines, and the opportunity to delve into emergency medicine (EM) opportunities early through an emergency medicine interest group (EMIG). For international medical graduates (IMGs) and orphan programs, in particular, these issues caused significant anxiety. Many students were unable to secure away rotations and/or receive the much-needed standard letter of evaluation (SLOE), which most program leadership teams deem necessary to a successful EM residency application. As such, these factors may have additionally led to far fewer IMG EM applicants.
According to AAMC’s Preliminary ERAS residency statistics from 2022, the overall number of applicants to EM decreased for the first time in over five years. However, the sole contributor to this general decline came from IMG applicants, who decreased from 19,259 in 2021 to 17,840 in 2022 (AAMC. 2022). This negative difference over one year was in sharp contrast to both MD and DO applicants, who increased in applications to EM within the same period. Given the data and anecdotal reports from international EMIGs, the questions raised are:
- Has the fear, or sheer inability, to secure an EM rotation and receive a SLOE been a prime contributor to a decrease in IMG EM residency applications?
- Did the impact of the pandemic on international students lead to a lack of advocacy for EM applicants and thus fewer applications to EM?
While aspects of these questions may be challenging to answer sufficiently without more data, we will reflect on some of the challenges IMG applicants face and routes to improve their experience.
With the COVID-19 pandemic causing medical schools to shift from in-person learning to online-based instruction during the peak of the virus, international EMIGs were forced to adapt to a platform not conducive to practical education. Some EMIGs revised previously face-to-face workshops into online instruction, teaching intravenous insertion, airway management, and EKG interpretation via Zoom-based flipped-classroom lectures. However, those EMIGs with less support, or those only recently formed, were forced to collapse until medical schools returned to on-campus instruction due to a lack of funding and institutional support. Because of the significant support international EMIGs have in advocating for EM, many students interested in the specialty may have been ill-prepared for the specific nature of the application if a primary advisor was not provided during medical school. This includes familiarizing students with the significant importance of the SLOE, how to schedule an EM rotation as an IMG or student from an orphan program, and priming students practically for an EM rotation through workshops and presentations. Furthermore, IMG students who did not have a home institution may have had unprecedented difficulties or limitations in obtaining rotations; this may have occurred due to various issues, including university policies on rotating away students and travel bans.
With a return to in-person learning, it will be of vital interest to see if the decrease in EM residency applications returns to a pre-pandemic figure for the IMG community. However, it is of utmost importance that those previously successful in navigating the EM residency application cycle support their medical schools’ EMIG, thus ensuring students interested in EM are prepared to adapt accordingly to the requirements that seem to change year-to-year for this population. Additionally, support from EM organizations for IMG applicants will also help increase education and resources for the students.
Impacts of the COVID-19 pandemic have not just affected IMGs, but the entire EM society, and students have been forced to adapt to an ever-changing residency application cycle. Based on EM residency application trends and feedback from international EMIGs, we have laid out numerous possibilities into why a down-trend in IMG applications may have occurred. These include difficulties securing an EM rotation, receiving a SLOE, and a lacking for EMIG endeavors leading to less interest in the specialty. We hope that with a slow return to pre-pandemic conditions globally, an up-trend in IMG applications to EM will also occur. It will be the mentoring and advocacy from the EM community as a whole that will support a return to normalcy, not just for IMG applications to EM and support for EMIGs, but the specialty in general.
References:
AAMC. 2022. ERAS Statistics. [online] Available at: https://www.aamc.org/data-reports/interactive-data/eras-statistics-data [Accessed 3 March 2022].
Related Content


May 02, 2023
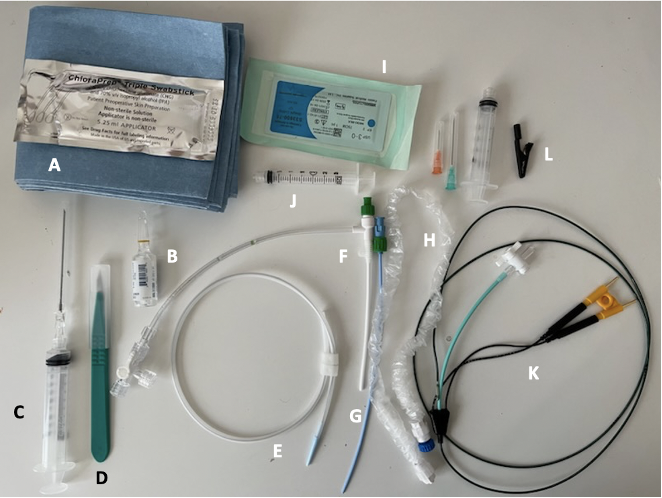
Critical Care Device Series: Transvenous Pacemaker
Temporary transvenous pacing (TTVP) utilizes central venous access to pass an electrode into the right ventricle. TTVPs are one of the most infrequently performed procedures by emergency physicians; however, it is essential for those working in any setting with critically ill patients to be well-equipped to perform this procedure emergently.




