Esophageal rupture is a rare condition that is recognized as one of the most fatal gastrointestinal injuries.
Time to diagnosis is an independent predictor of mortality in acute esophageal rupture making this a can’t miss diagnosis for emergency physicians. Here, we describe a rare presentation of Boerhaave syndrome and the utility of ultrasound in the diagnosis.
Case
A 41-year-old female with a history of congenital CMV, developmental delay, VSD, esophageal stricture, and episodes of food impaction presented to the emergency department with symptoms of abdominal pain and nausea. The patient reportedly complained of achy non-radiating epigastric pain and nausea after choking on mashed potatoes the night before. Overnight her symptoms persisted gradually involving upper back pain and chest pain, prompting ED evaluation. The patient denied fever, chills, or vomiting.
On arrival, the patient was afebrile with a BP 96/60, HR 134, RR 24, and oxygen saturation 94% on room air. Chest X-ray was concerning for bilateral pleural effusions and possible infiltrate. Labs showed Na of 134 mmol/L, CO2 of 18 mmol/L, anion gap of 19 mmol/L, lactic acid of 7.2 mmol/L, troponin of .046 ng/mL, WBC 29.3 K/uL, and hemoglobin of 10.8 g/dL. The patient was given ampicillin/sulbactam and 2 L of normal saline.
She was transferred to the ICU with a working diagnosis of aspiration pneumonia.
On arrival to the ICU, the patient was ill-appearing with improved blood pressure but worsened dyspnea and hypoxemia. Physical exam was significant for increased work of breathing, diaphoresis, cold extremities, and delayed capillary refill. Chest X-ray was unchanged from earlier. Antibiotics were broadened and BiPAP initiated. Due to concern for cardiogenic shock a bedside ultrasound was performed. The cardiac ultrasound appeared distorted: a rightward-deviated cardiac silhouette, a seemingly large pericardial effusion, and a hyperechoic fluctuant mass on the pericardium (Image 1).
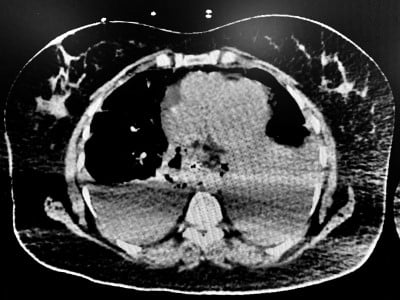
Due to the unusual anatomy it was difficult to determine whether the fluid was a pericardial effusion or a pleural effusion. Echo findings were discussed with the cardiology team and the decision was made to perform a thoracentesis and reassess clinical status. A left-sided thoracentesis drained murky brown pleural fluid. During the procedure, the patient began vomiting and became acutely hypoxic requiring intubation for airway protection. Based on the appearance of the pleural fluid, persistent pericardial effusion on repeat ultrasound, and development of chest wall crepitus the patient was sent for CT imaging for suspected esophageal injury. CT of the chest showed air within the subcutaneous tissue and mediastinum suspicious for acute esophageal rupture (Image 2).

Diagnosis
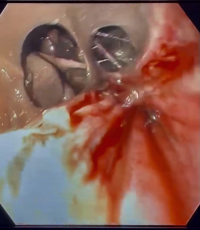
Cardiothoracic surgery was consulted and the patient was immediately taken to the OR for Esophagogastroduodenoscopy and esophageal repair. A 10 cm esophageal tear was identified intraoperatively (Image 3).
Discussion
Although the most common cause of esophageal rupture is iatrogenic, accounting for nearly 85% of reported cases, spontaneous rupture is the second most common cause.1 Boerhaave syndrome, first described by Herman Boerhaave in 1724, is a spontaneous transmural perforation of the esophagus usually due to forceful emesis.1 Other less common culprits are trauma, defecation, seizures, childbirth and weightlifting.1
A common algorithm used to diagnose Boerhaave syndrome is Mackler’s triad: vomiting, chest pain, and subcutaneous emphysema. Unfortunately, only 14% of patients with Boerhaave syndrome present with this classic triad.2 Delayed and sometimes missed diagnosis can occur, often due to non-specific and vague clinical presentation as seen in this case.
Case Conclusion
Our case presents an unusual presentation of Boerhaave syndrome. Not only did our patient's symptoms begin after eating soft food, but emesis and development of crepitus was a very late finding. Another layer of complexity came from the inability of the patient to provide a history herself secondary to her cognitive disability due to congenital CMV. However, this case demonstrates the importance of a high index of suspicion in patients with symptoms after choking. Although aspiration pneumonia is more common, esophageal injury should remain high on the differential especially in the setting of worsening respiratory status and overall patient decline. Another important aspect of this case is the importance of thorough chart review, which in our patient unveiled her history of esophageal stricture.
Lastly, CT imaging and esophagography have proven utility when diagnosing esophageal perforation, however emergency ultrasound is a fast, portable and non-invasive imaging modality that can aid diagnosis. Ultrasound is routinely used by emergency physicians, primarily in those presenting with undifferentiated shock. Although ultrasound findings are not highly specific, when coupled with a high index of clinical suspicion it can be used to support diagnosis and expedite surgical intervention in patients with acute esophageal rupture.
References
- Triadafilopoulos G. Boerhaave syndrome: Effort rupture of the esophagus. Uptodate. https://www.uptodate.com/contents/boerhaave-syndrome-effort-rupture-of-the-esophagus?search=esophageal+rupture&source=search_result&selectedTitle=1~38&usage_type=default&display_rank=1. Published February 25, 2020. Accessed August 5, 2021.
- Turner AR, Turner SD. Boerhaave syndrome. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK430808/. Published January 1, 2021. Accessed August 5, 2021.



