Sick sinus syndrome, rather than being a single specific disease, is a collection of disorders that add up to trouble for the sinus node.
A 78-year-old female with history only of leg edema presents to the ED complaining of nausea
and dizziness for the past few hours. EMS reports that upon their arrival she was found to be in atrial fibrillation and subsequently passed out, at which time she was noted to have an asystolic episode of about 4.5 seconds, which self-resolved. Upon arrival to the ED she is noted to be in atrial fibrillation at a rate of 110-120 with a blood pressure of 101/60, complaining of pain of chest and abdomen and dry heaving. Moments later her heart rate decreases significantly, rhythm noted to be a complete heart block followed by asystole (Figure 1); she is unresponsive at this time. Seconds later she is again awake and alert, now sinus rhythm in 80s. The decision is made to place an emergent transvenous pacemaker.
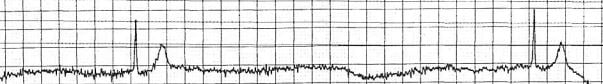
Figure 1. Pause of about 4.5 seconds
Sick sinus syndrome (SSS) is a collection of disorders in which the heart does not successfully perform its pacemaking function.1 This syndrome is diagnosed based on electrocardiographic findings of arrhythmia, such as bradyarrhythmia or sinus pause. It is often associated with clinical signs and symptoms including fatigue, lightheadedness, presyncope, syncope, dyspnea on exertion, chest discomfort, or palpitations.2 It is a fairly common condition, particularly in elderly patients with concomitant cardiac disease, and prevalence is high in patients who have an increased BMI or a history of hypertension, diabetes, coronary artery disease, or heart failure.
About half of patients with SSS will have a tachycardia- bradycardia syndrome in which they have a rapid heart rate, often atrial fibrillation or atrial flutter, followed by bradyarrhythmia.3 The incidence of SSS increases with age and affects males and females similarly. With an increase in our geriatric population, the prevalence of SSS in the United States is expected to double in the next 50 years.4
Sinus node dysfunction may be related to atrial remodeling secondary to aging, heart failure, or atrial fibrillation, or it may be genetic and secondary to ion channel dysfunction. Infiltrative processes or ischemia stemming from coronary artery disease can also affect the function of the sinus node.3 Medications that affect the atrioventricular node such as beta blockers, calcium channel blockers, digoxin, antiarrhythmics, and acetylcholine esterase inhibitors should be considered as reversible causes of sick sinus syndrome,2 as should electrolyte abnormalities, hypothyroidism, hyperthyroidism, hypoxia, hypothermia, and toxins.1
After ruling out secondary causes including cessation of nonessential medications and monitoring for clearance through 3-5 half lives,5 SSS in patients with clinical symptoms should be treated by placement of a permanent pacemaker.3 In the acute setting, any unstable patient presenting with findings consistent with SSS should be treated by standard ACLS, considering atropine but not delaying initiation of pacing. Transcutaneous pacing is a temporizing measure while arranging to place a transvenous pacemaker. Those who are stable should be monitored with transcutaneous pads in place while arranging definitive care.5
Approximately 30-50% of the pacemakers placed in the United States are for the treatment of SSS.3 Pacemakers have not been shown to reduce mortality in SSS but are associated with decreased symptoms and improved quality of life.1
A prospective multicenter study that examined the 12 months before and after pacemaker placement in 87 patients found a significant decrease in symptoms including syncope and dizziness after pacemaker placement as well a significant decrease in number of falls.6 There is a high incidence of atrial fibrillation in patients with SSS requiring pacemaker, so thrombotic risk must be considered and anticoagulation initiated as indicated.3,5
Case Conclusion
A transvenous pacemaker was successfully placed and the patient was admitted to the cardiac intensive care unit. She was noted on echocardiogram to have a severely dilated left atria with mild diastolic dysfunction. A permanent pacemaker was placed, and she was discharged on apixaban.
References
1. Semelka M, Gera J, Usman S. Sick Sinus Syndrome: A Review. Am Fam Physician. 2013;87(10):691-696.
2. Homoud MK. Sick sinus syndrome: Clinical manifestations, diagnosis, and evaluation. Post TW, ed. UpToDate. Waltham, MA: UpToDate Inc.
3. Walsh-Irwin C, Hannibal GB. Sick Sinus Syndrome. AACN Adv Crit Care. 2015;26(4):376-380.
4. Jensen PN et al. Incidence of and Risk Factors for Sick Sinus Syndrome in the General Population. J Am Coll Cardiol. 2014;64(6):531-538.
5. Homoud MK. Sick sinus syndrome: Treatment. Post TW, ed. UpToDate. Waltham, MA: UpToDate Inc.
6. Brenner R et al. Reductions of Falls and Fractures after Permanent Pacemaker Implantation in Elderly Patients with Sinus Node Dysfunction. Europace. 2017;19(7):1220-1226.



