2020 marked the first year of the new unified residency match, and the data is here. How has the merger of the ACGME and AOA paths to accreditation affected osteopathic candidates?
2020 marked the first year of the new unified residency match, and the data is here. Before the single GME accreditation system, osteopathic medical students applying for emergency medicine had two separate matches they could participate in: the AOA (osteopathic) or the ACGME (allopathic) match. For osteopathic students, this posed additional challenges in developing an application strategy. These students had to decide whether to participate in one or both matches, which created a complicated series of potential match outcomes and extra financial burden. Currently, the ACGME now serves as the sole accrediting institution for residencies and fellowships, and all MD and DO students applying for emergency medicine will participate in the same single match.
Throughout the 5-year transition process, 98% of AOA accredited programs that applied have received ACGME accreditation, and 233 programs (spanning 27 specialties) have received "Osteopathic Recognition." This includes 40+ emergency medicine programs with 5 programs maintaining "Osteopathic Recognition." NRMP data shows that the match rate for DO graduates was 90.7%, and the total GME placement rate in the combined match this year was an impressive 99.2%. This is a significant increase in both match and placement rate despite increasing 1,103 osteopathic applicants from 2019. The goal of this article is to explore this data as it relates to matching emergency medicine as an osteopathic applicant and how it compares to prior years. We believe this analysis will set a new framework for assessing competitiveness and developing application strategies for osteopathic medical students applying for emergency medicine.
2020 Osteopathic Charting Outcomes Data
So osteopathic applicants match better in the ACGME match than in any year prior, but how about for emergency medicine specifically? When comparing the NRMP Osteopathic Charting Outcomes data from this year and 2018 (this data is released every other year), the overall match rate has stayed the same: 83.8% (643/767) in 2020 and 83.9% (434/517) in 2018. Due to the AOA match in 2018, it is difficult to assess the real increase in the number of osteopathic EM applicants and matches for 2020. Though 250 more osteopathic students applied EM in the ACGME match in 2020 than in 2018, it is essential to note that the 180 applicants applied EM in the AOA match that year. Of all matched osteopathic students in 2020, 12.3% matched into emergency medicine. For comparison, the match rate in emergency medicine for US MDs this year was 91.9% (1,739/1,598). This indicates that though the DO bias is dissipating, it still exists and should be considered when applying and evaluating your specialty's competitiveness.
Of note is the increase in the percentage of Program Directors who report their willingness to interview and rank DO applicants. In the 2020 NRMP Program Director Survey, 74% of EM PDs reports that they "often interview" DO applicants, which is an increase of 14% from 2018. Likewise, 78% of EM PDs report they "often rank" DO applicants (an increase of 16% from 2018). Part of this increase is likely explained by the addition of former AOA EM programs into the survey this year.
USMLE/COMLEX Scores
In 2020, the mean USMLE Step I and COMLEX Level I score for osteopathic applicants that matched EM successfully were 228 and 562, respectively. The mean USMLE Step I and COMLEX Level I score for an unmatched osteopathic applicant were 219 and 504. The mean USMLE Step 2 and COMLEX Level II score for matched applicants was 241 and 599, while the mean for unmatched applicants was 231 and 532. Though the overall match rate for osteopathic students is 83%, one can better determine their chance of a successful match looking at the board score specific data (Figure 1). The NRMP also has an "Interactive Charting Outcomes" that allows you to visualize match data in greater detail with more parameters.
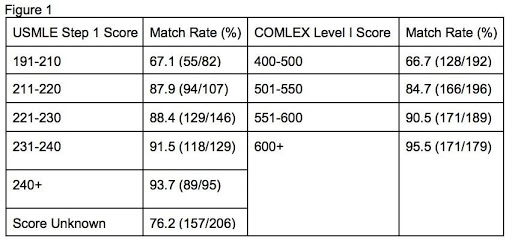
Those in the category of "Score Unknown" are presumably applicants who did not take the USMLE or did not disclose their score to the NRMP. Though it is possible to match without a USMLE score as an osteopathic applicant, currently, it is still primarily advised to take the USMLE. A survey conducted by the CORD Advising Students Committee for Emergency Medicine showed that of the programs that consider osteopathic applicants, only half would offer an interview without USMLE Step 1 and Step 2. In contrast, 87% would offer an interview with an applicant who had taken USMLE Step 1. Also of note is that 27% of program directors surveyed do not weigh the COMLEX at all.
It is important to note that the USMLE Step 1 exam score will transition to being reported as Pass/Fail no earlier than January 1, 2022. This means that extrapolating current match data related to specific USMLE Step 1 Scores may be futile. However, the USMLE Step 2 CK and COMLEX Level 1 exam (as of the publication date of this article) will remain to be scored in the traditional 3-digit fashion. So this data is still of value when comparing those exam scores to previous match outcomes for applicants applying in 2022 and beyond.
How many Interviews/Ranks?
The topic of "how many interviews needed to match" is a hot topic; however, the data on this has been relatively consistent for osteopathic applicants. This year, osteopathic applicants ranked between 9-12 emergency medicine programs had a match rate of 95.8%, with quickly diminishing returns after ten interviews. Due to the COVID-19 pandemic and the resulting changes to the 2020-2021 application cycle, specifically adopting all virtual interviews and restrictions on away rotations, it remains to be seen if these numbers will hold. However, the CORD Consensus Statement currently recommends attending 12 interviews with an absolute maximum of 17 for the 2020-202 application cycle.
Geographic considerations
One factor that may influence application strategies for osteopathic applicants is the geographic match distribution for DOs. Unsurprisingly, DO matches are greater in states with a larger number of previously AOA accredited programs (ie, OK, MI, PA, OH). However, this is not always the case (ie, NY, NJ, IL, FL). Of the 35 states (including the District of Columbia) with an EM residency program, 21 (60.0%) filled 20% or more spots with DO applicants last year. This includes three states (NV, OK, WV) that each matched >50% DO applicants to available positions. These states comprise the majority of EM residency positions, with 1,382 available in 2020 compared to only 160 open positions in the ten states where 0-5% of matched EM applicants came from DO programs.
Using the Mississippi River as a divider of East and West, most EM programs, and thus residency positions, are located in the East. There were 1,825 positions available in the East compared to 564 in the West in 2020. DO applicants filled 551 (30.2%) of available East positions versus 131 (23.2%) West positions. Of note, there are currently 37 osteopathic medical schools offering instruction at 58 campuses. Thirty-five (39.7%) of these campuses are located in the West. Of the five programs with Osteopathic Recognition, two are located in the West, both at Oklahoma State University affiliated programs.
States in which 20% or more of EM spots were filled with osteopathic graduates
Arizona (16/49 – 32.7%)
Missouri (10/47 – 21.3%)
Oklahoma (27/35 – 77.1%)
Delaware***(3/12 – 25%)
Nebraska*** (4/11 – 36.4%)
Pennsylvania (84/202 – 41.6%)
Florida (54/185 – 29.2%)
Nevada (17/27 – 63%)
South Carolina (18/45 – 40%)
Georgia (10/50 – 20%)
New Jersey (39/88 – 44.3%)
Texas (32/137 – 23.4%)
Kansas***(2/10) – 20%)
New York (92/372 – 24.7%)
Utah*** (4/9 – 44.4%)
Michigan (101/228 – 44.3%)
North Carolina (16/79 – 20.3%)
Virginia (16/50 – 32%)
Mississippi (9/22 – 40.9%)
Ohio (54/141 – 38.3%)
West Virginia (14/24 - 58.3%)
States in which 0-5% of EM spots were filled with osteopathic graduates
Arkansas (0/16)
Vermont*** (0/6)
New Mexico*** (0/12)
Colorado*** (0/17)
Washington*** (0/12)
Wisconsin (1/24 – 4.2%)
D.C. (0/21)
Maryland (1/24 – 4.2%)
New Hampshire*** (0/6)
Rhode Island (1/22 - 4.5%)
Others
California (29/229 – 12.7%)
Illinois (24/135 – 17.8%)
Kentucky (2/29 - 6.9%)
Tennessee (2/18 - 5.9%)
(States in which the majority of EM spots were filled with osteopathic graduates in red.)
(*** indicates states that only have 1 EM residency. It does not include military matches.)
Strategies
Taking all of these things into consideration, there are many areas that each osteopathic student must consider once they have decided to apply for EM residency. First, you must determine what type of training you desire (county, academic, community, hybrid) and then assess your relative competitiveness at programs in each of those categories. Another consideration is whether to apply to any of the 5 programs that currently maintain Osteopathic Recognition.
Historically, competitiveness has been heavily assumed to be related to board exam scores, with many programs focusing on USMLE Step 1 scores. However, with Step 1 going to pass/fail as early as 2022, there will likely be a shift of focus to Step 2 and possibly even COMLEX Level 1/2 for osteopathic students as long as they continue to report scores in the 3-digit format. Recall though, based on the PD Survey, the SLOE remains the most heavily weighted aspect of any EM applicant's application.
When applying for EM residencies, osteopathic students also should consider geographic location. As previously mentioned, most PGY-1 EM residency positions (76.4%), especially those currently occupied by DOs, are located east of the Mississippi River. DOs do, however, now makeup>20% of PGY-1 positions in 21 states. One strategy osteopathic applicants might consider is to research geographic regions and the programs that have historically matched DO candidates. This information can be found on both EMRA Match or the individual programs' websites.
Conclusions
Osteopathic applicants who are developing an application strategy for emergency medicine residency should first assess their relative competitiveness with metrics such as board scores. Applicants applying with a 3-digit USMLE Step 1 score can use the data and diagrams in this article to obtain an idea of their competitiveness. Future applicants should consider taking both the USMLE and COMLEX with particular focus on the USMLE Step 2 exam as it will remain scored. Those with below-average USMLE scores or no USMLE score should focus their applications towards the historically AOA program and those with osteopathic recognition, as these programs are more familiar with using the COMLEX as their primary metric. Targeting programs in states with a broad representation of DOs may increase the interview return and match success. Most importantly, board scores are not the end-all-be-all, and the primary focus should be on performing well on your emergency medicine rotations to obtain good SLOEs. The EMRA Match map is a useful resource to quickly identify programs with DO representation, score cutoffs, and programs that accept the COMLEX.
References
- National Resident Matching Program. Charting Outcomes in the Match: Senior Students of U.S. DO Medical Schools. 2nd ed. Available at: https://mk0nrmp3oyqui6wqfm.kinstacdn.com/wp-content/uploads/2020/07/Charting-Outcomes-in-the-Match-2020_DO-Senior_final.pdf. Accessed September 20, 2020.
- ACGME, AOA, and AACOM Usher in New Era of Single Accreditation for Graduate Medical Education. Accreditation Council for Graduate Medical Education website. Updated on July 1, 2020. Accessed September 20, 2020. https://www.acgme.org/Newsroom/Newsroom-Details/ArticleID/10568/ACGME-AOA-and-AACOM-Usher-in-New-Era-of-Single-Accreditation-for-Graduate-Medical-Education
- 1 in 4 U.S. medical students attends an osteopathic medical school. American Osteopathic Association website. Updated 2020. Accessed October 13, 2020. https://osteopathic.org/about/affiliated-organizations/osteopathic-medical-schools/
- EMRA Match. Emergency Medicine Residents’ Association website. Accessed October 13, 2020. https://webapps.emra.org/utils/spa/match#/search/map
- Consensus Statement on the 2020-2021 Residency Application Process for US Medical Students Planning Careers in Emergency Medicine in the Main Residency Match. Council of Residency Directors in Emergency Medicine website. Updated 2020. Accessed September 20, 2020. https://www.cordem.org/siteassets/files/2020-res-app-consensus-statement-v2.pdf



