ARTICLE: Møller JE, Engstrøm T, Jensen LO, et al., for the DanGer Shock Investigators. Microaxial Flow Pump or Standard Care in Infarct-Related Cardiogenic Shock. N Engl J Med. 2024;390(15):1382-1393.
OBJECTIVE
To assess the efficacy of the microaxial flow pump, namely the Impella CP made by Abiomed, in the treatment of patients with STEMI and cardiogenic shock and planned revascularization
BACKGROUND
Cardiogenic shock is defined as a state of tissue hypoperfusion and end-organ dysfunction owing to a primary cardiac disorder with low cardiac output (CO) that can present in different stages.1 This is often precipitated by an acute ST segment elevation myocardial infarction (STEMI). Standard intervention for STEMI with cardiogenic shock includes early revascularization via percutaneous coronary intervention (PCI) or bypass grafting. Even after revascularization, cardiogenic shock develops in approximately 8-10% of patients and carries a mortality of 40-50%.2,3
Mechanical circulatory support (MCS) devices were developed to help increase CO for patients in low-output states, including those in cardiogenic shock. The end goal of MCS varies, but it can act as a bridge to recovery for patients with acute MI both before and after revascularization. MCS devices include ventricular assist devices (VADs), extracorporeal membrane oxygenation (ECMO), microaxial flow pumps (Impella), intra-aortic balloon pumps (IABPs), and various iterations of these. There is growing evidence that MCS can provide myocardial protection and improve myocardial recovery in acute coronary syndromes.1
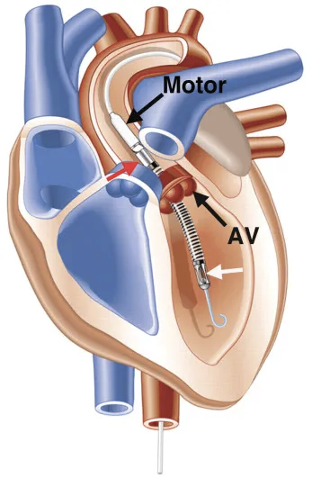
One MCS device known as an Impella is a microaxial flow pump that moves blood from the left ventricle to the ascending aorta through a catheter (Figure 1). The Impella CP, the device used in this study, provides a maximum average flow of 3.7 L/min.4 From a physiological standpoint, this provides increased CO, increased coronary perfusion, and decreased myocardial oxygen demand. Impellas can be placed surgically or percutaneously and, based on the device used, can provide either right or left ventricular support. Some advantages are that Impellas can provide moderate support and have an inherently simpler and less invasive design than other forms of MCS. They can be placed in the cardiac catheterization lab before or after revascularization.
Despite the relative ease of insertion and resultant increase in CO, trials have not shown definitive benefit for Impellas in patients experiencing acute MI with cardiogenic shock. The PROTECT II study did not find a difference between Impella and IABPs for patients undergoing high-risk PCI. However, the Impella did show favorable hemodynamic support.5 Three additional smaller RCTs did not show a clinical benefit of Impellas over/with IABPs in patients experiencing acute MI and cardiogenic shock.6
The Danish-German Cardiogenic Shock (DanGer Shock) trial looks at a specific patient population experiencing cardiogenic shock due to acute STEMI to determine if the use of a microaxial pump (Impella) improves mortality over standard guideline-directed therapies. The study also looks at various secondary end-points and adverse events which are typically higher in patients with MCS.
Figure 1. Impella Schematic
DESIGN
This trial was an international prospective multicenter randomized open label trial. The trial was initially intended to be only conducted in Denmark with the first patient being enrolled in January 2013. However, due to slow enrollment, the trial was expanded to include participants in Germany and UK in 2019 and 2021, respectively.
The trial protocol was approved by an institutional ethics committee at each participating site, and an independent data and safety monitoring committee oversaw patient safety in the trial and performed a formal interim analysis after the enrollment and complete follow-up of 180 patients. The trial itself was funded by the Danish Heart Foundation and Abiomed, but no trial funders took part in the trial design, nor did they participate in the analysis or interpretation of collected data.
The study enrolled participants 18 years or older who presented with STEMI and signs and symptoms of cardiogenic shock as defined by the authors. Patients underwent randomization either before or up to 12 hours after catheterization and received vasopressor support if indicated. In the group receiving the microaxial flow pump this was placed immediately following randomization and was set to run at its highest setting for a minimum of 48 hrs unless complications arose. In the presence of continued hemodynamic instability, therapy could be escalated to an Impella 5.0, Impella RP, or ECMO. In the standard group, should hemodynamic instability persist, it was recommended physicians place the patient on ECMO; however, an Impella 5.0 was permitted. If a patient in the standard therapy group received an Impella CP for hemodynamic support this was considered to be a protocol violation.
INCLUSION CRITERIA
At least 1 of 3 combinations of presentations:
- STEMI and cardiogenic shock
- ST segment elevation myocardial infarction of less than 36 hrs duration, confirmed by new-onset ST segment elevation
- Presence of cardiogenic shock for < 24 hrs defined as: peripheral signs of tissue hypoperfusion such as arterial blood lactate ≥2.5 mmol/L and/or SvO2<55% with a normal PaO2 and systolic blood pressure < 100mmHg and/or need for vasopressor therapy
- LVEF < 45%
- STEMI equivalent and cardiogenic shock
- ECG with new-onset ST segment depression or left bundle branch block of < 36 hrs duration and emergency angiography demonstrating acute proximal occlusion of coronary artery
- Presence of cardiogenic shock of < 24 hrs defined as: peripheral signs of tissue hypoperfusion such as arterial blood lactate ≥2.5 mmol/L and/or SvO2<55% with a normal PaO2 and systolic blood pressure < 100mmHg and/or need for vasopressor therapy
- LVEF < 45%
- STEMI, where shock develops during or up to 12 hrs after revascularization
- Patients with STEMI of < 36 hrs duration treated with primary percutaneous intervention that develop cardiogenic shock, according to the above definition, during or within 12 hrs of intervention are also eligible.
EXCLUSION CRITERIA
- Shock duration > 24 hrs
- Non-cardiogenic etiology of shock
- Shock secondary to a mechanical complication of MI: rupture of a papillary muscle ventricular free wall or ventricular septum
- OHCA with persistent GCS <8 (Note: cardiac arrest in the ambulance or cardiac arrest with GCS <8 did not preclude enrollment in the study)
- Evidence of severe RV failure defined as: a right ventricle exceeding the size of the LV in apical four-chamber view, TAPSE < 1 cm, and septal shift
- Severe aortic valve regurgitation or stenosis
- Severe peripheral arterial disease preventing Impella placement
- Mechanical aortic valve
- Aortic valve anatomy preventing Impella placement
- LV thrombus
- Infective endocarditis
- Life expectancy < 1 yr secondary to medical comorbidities
- Language barrier or mental disorder preventing informed consent
PRIMARY AND SECONDARY OUTCOMES
Primary: all-cause mortality at 180 days
Secondary:
- Composite cardiac end-point consisting of 1) the need for addition of alternate mechanical circulatory support devices or cardiac transplant or 2) all-cause death, whichever came first
- Hospital-free days alive from discharge to 180-day follow up
Adverse events were additionally tracked in the following categories: bleeding, limb ischemia, cerebrovascular accident, need for renal replacement therapy, sepsis with confirmed bacteremia, device failure, and worsening of aortic insufficiency.
KEY RESULTS
More than 1,200 patients were screened across 14 European centers throughout the enrollment period, of whom 360 were enrolled. After excluding 5 patients for whom consent could not be obtained, a total of 355 patients were included in the final analysis (179 in the Impella group and 176 in the standard care group).
The Impella CP was successfully implanted in 170 of the 179 patients (95.0%) randomized to receive it after 3 patients crossed over to the control group and 6 failed placement attempts. Three of the 176 patients in the standard care group (1.7%) crossed over to the Impella group during the study.
All-cause mortality at 180 days was 45.8% for patients in the Impella group and 58.5% in the standard care group (HR 0.74; 95% CI 0.55-0.99; P = 0.04). The number needed to treat with Impella in order to avoid 1 death was 8. Patients in the Impella group required escalation of treatment to a more advanced mechanical circulatory support system (Impella 5.0, Impella RP, or ECMO) in 15.6% of patients in the Impella CP group versus 21.0% of patients in the standard care group. While not statistically significant, there was a trend toward more days alive and out of the hospital in the Impella group, with this group having a mean of 82 such days and the standard care group having a mean of 73. Interestingly, subgroup analyses demonstrated the association with Impella and significantly improved survival was seen in male but not female patients. The mortality benefit was most notable in patients with significant hypotension (MAP <63 mmHg versus >63 mmHg) and in those with multivessel CAD versus single vessel disease.
Slightly more than half of the Impella group (52.5%) experienced a composite cardiac end-point event (including need for escalation to additional mechanical circulatory support, cardiac transplant, or death), while 63.6% of standard care patients had an event (HR 0.72; 95% CI 0.55 to 0.95). The number needed to harm for the Impella group was 6, with listed adverse events of bleeding, limb ischemia, or renal replacement therapy significantly higher than the standard therapy group, 24.0% vs. 6.2%, respectively (RR 4.74; 95% CI 2.36 to 9.55). It should, however, be noted that these are all expected complications with mechanical circulatory support regardless of the device being used.
LIMITATIONS
Because of the strict inclusion criteria as well as the general lack of heterogeneity within the study population, this study does present questions regarding generalizability of results. Nearly 80% of the participants were males and likely predominantly white based on the local population, highlighting the need for future studies with a more heterogeneous patient population before broader recommendations may be made for patients presenting with acute MI-associated cardiogenic shock. It is also important to note that the study excluded patients without STEMI, those with GCS <8 following cardiac arrest, cases of predominantly biventricular failure, and those with SCAI stage C shock without elevated serum lactate. While this is not necessarily a limitation as it demonstrates appropriate selection of patients who are likely to benefit most from a device that introduces some inherent risk, it is a reminder that patients should be screened for candidacy prior to consideration of implantation and results of this study should not be generalized to inappropriately selected patients.
Another limitation of the study was the time period of enrollment. It took 10 years to enroll the study population, during which time there were presumably advances in practice. Additionally, the centers involved in the study had high capabilities for and experience with MCS. It remains unclear at this point how such devices would perform in less experienced centers.
Finally, the study compared outcomes at 180 days, which leaves questions about implications on long-term mortality. Some complications of MCS, such as limb loss and dialysis dependency, may well impact longer-term mortality and morbidity in a way that was not captured in this study.
Overall, this is a very well-done study that provides long-anticipated answers to pivotal questions about the care of critically ill ACS patients suffering from cardiogenic shock. The authors were able to demonstrate mortality benefit of Impella CP in these patients when appropriately screened for device candidacy. While further studies are required to build upon this data and improve generalizability, this study represents a valuable contribution to the current literature on the topic.
EM/CCM TAKE-AWAYS
- In this randomized control trial, the use of a microaxial flow pump (Impella CP) in acute MI complicated by cardiogenic shock significantly improves survival when compared to standard guideline-directed therapies. This study provides promising evidence for Impella use in acute MI-associated cardiogenic shock.
- The Impella group was associated with an increased adverse events rate and increased need for renal replacement therapy when compared to the standard care group, consistent with known risks of all mechanical circulatory support devices.
- Patients with multivessel CAD and more severe hypotension achieved greater benefit from an Impella than those with single-vessel disease and MAP >63 mm Hg respectively.
- Cardiogenic shock is a complex pathology with multiple etiologies, treatments, and a difficult-to-study patient population. Further studies will be needed to provide definitive guidelines around MCS in specific populations.
- Emergency medicine physicians must become familiar with the different types of MCS and patients presenting with cardiogenic shock as we will encounter them in the ED and throughout the hospital. Identifying patients who may be candidates for such devices early may positively impact their clinical course.
REFERENCES
- Bernhardt AM, Copeland H, Deswal A, et al. The International Society for Heart and Lung Transplantation/Heart Failure Society of America Guideline on Acute Mechanical Circulatory Support [published correction appears in J Heart Lung Transplant. 2023 Dec;42(12):1770]. J Heart Lung Transplant. 2023;42(4):e1-e64.
- Helgestad OKL, Josiassen J, Hassager C, et al. Temporal trends in incidence and patient characteristics in cardiogenic shock following acute myocardial infarction from 2010 to 2017: a Danish cohort study. Eur J Heart Fail. 2019;21(11):1370-1378.
- Jentzer JC, van Diepen S, Barsness GW, et al. Cardiogenic Shock Classification to Predict Mortality in the Cardiac Intensive Care Unit. J Am Coll Cardiol. 2019;74(17):2117-2128.
- Zein R, Patel C, Mercado-Alamo A, Schreiber T, Kaki A. A Review of the Impella Devices. Interv Cardiol. 2022;17:e05.
- O'Neill WW, Kleiman NS, Moses J, et al. A prospective, randomized clinical trial of hemodynamic support with Impella 2.5 versus intra-aortic balloon pump in patients undergoing high-risk percutaneous coronary intervention: the PROTECT II study. Circulation. 2012;126(14):1717-1727.
- Møller JE, Engstrøm T, Jensen LO, et al., for the DanGer Shock Investigators. Microaxial Flow Pump or Standard Care in Infarct-Related Cardiogenic Shock. N Engl J Med. 2024;390(15):1382-1393.