Pneumocephalus is a condition that is defined as air present in the intracranial space.
The disease process is usually seen in patients with disruption of the skull and is a rare finding in the absence of prior neurosurgical intervention or trauma.1
Cases of pneumocephalus in the absence of trauma have been published in case reports and include underlying etiologies such as pneumococcal meningitis, CSF leaks, and epidural blocks.2 Patients with pneumocephalus can have a wide-ranging presentation from benign to respiratory arrest,3 with the most common presenting complaint being headache.
This case highlights a unique finding of syncope being a presenting symptom of pneumocephalus, which has not been reported before.
Case Report
A 62-year-old female with a history of hypertension (HTN) and chronic shoulder pain presented to the emergency department for evaluation of syncope. The patient was getting an epidural steroid injection and immediately after the injection had a syncopal episode witnessed by office staff. The patient was caught by staff before falling to the ground. Upon EMS arrival, the patient was alert and oriented. Vitals at that time were notable for blood pressure (BP) 70/40 and heart rate (HR) of 40.
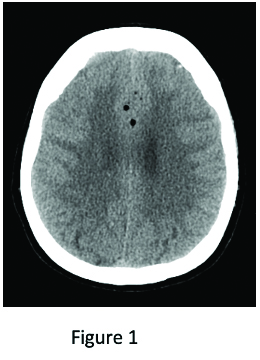
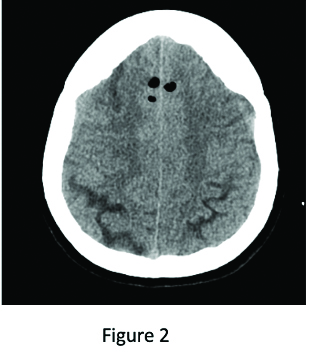
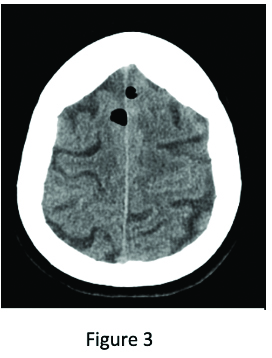
Upon presenting to the ED, the patient was mentating well, with vitals showing BP of 106/62 and HR of 68. The patient had no complaints aside from a headache that was currently resolving. A STAT EKG was obtained. It showed normal sinus rhythm at 69 beats per minute, with no acute ischemic changes. Labs were unremarkable. A chest X-ray (CXR) showed no radiographic evidence of acute pulmonary disease. Computed tomography (CT) of the head was performed (Figures 1, 2, and 3), which showed: “Numerous foci of pneumocephalus throughout the brain. Given the history or recent epidural steroid injection, findings may be related to injection of air into the thecal sac during the procedure. There is no significant mass effect of midline shift.”
The patient’s repeat neurological exam continued to be unchanged from initial baseline presentation. No focal deficits were noted, and the patient only complained of a headache. She remained vitally stable and was transferred to another institution for neurosurgical evaluation and management.
Discussion
Current reported cases of pneumocephalus due to epidural injections have shown that the most common presenting symptom in these patients is an intense headache.4 There is one case report that identifies respiratory arrest as the presenting symptom, showing that pneumocephalus can present with a wide range of neurological symptoms, from benign to life threatening.
Pneumocephalus is a known complication of accessing the epidural space. This can occur from air accidentally being injected into the intrathecal space when the “loss of resistance” technique is used to identify the epidural space.5 The presence of air in the epidural space can cause seizures by irritating the cerebral cortex.6
In our patient, it is plausible to assume that irritation of the cerebral cortex could have caused her to have a syncopal vs. seizure episode.
CT is the gold standard for diagnosing pneumocephalus and can detect as little as 0.55mL of intracranial gas. Treatment of pneumocephalus is usually conservative, with 85% of reported cases reabsorbing spontaneously without intervention during the first week of developing the condition.7
It is important to keep a high clinical suspicion in the appropriate clinical environment, as this is a rare complication in the non-traumatic setting, with the main barrier to diagnosis being a low index of suspicion. This case highlights the importance of early consideration, recognition, and treatment of pneumocephalus, especially given the low incidence rate and likelihood for atypical presentations outside of the traumatic setting.
References
- Schirmer CM, Heilman CB, Bhardwaj A. Pneumocephalus: Case Illustrations and Review. Neurocritical Care.2010;13(1):152-158.
- Reddi S, Honchar V, Robbins MS. Pneumocephalus associated with epidural and spinal anesthesia for labor. Neurology Clinical Practice. 2015;5(5):376-382.
- Barr DL, McDonald BS. Iatrogenic pneumocephalus following a cervical epidural steroid injection: A case report. Radiology Case Reports. 2021;16(12):3875-3878.
- Verdun AV, Cohen SP, Williams BS, Hurley RW. Pneumocephalus after lumbar epidural steroid injection: A case report and review of the literature. A & A Case Reports. 2014;3(1):9-13.
- Saberski L, Kondamuri S, Osinubi O. Identification of the epidural space: Is loss of resistance to air a safe technique? A review of the complications related to the use of air. Regional Anesthesia and Pain Medicine. 1997;22(1):3-15.
- Dabdoub CB, Salas G, Silveira E doN, Dabdoub CF. Review of the management of pneumocephalus. Surgical Neurology International. 2015;6(1):155.
- Penrose-Stevens A, Ibrahim A, Redfern RM. Localized pneumocephalus caused by Clostridium perfringens meningitis. British Journal of Neurosurgery. 1999;13(1):85-86.



