
POCUS is a key diagnostic tool that can allow emergency physicians to diagnose a range of injuries. This case illustrates the utility of POCUS in managing a case of necrotizing fasciitis in the emergency department.
Faculty editor: Kaylah Maloney, MD
EMRA Ultrasound Committee editor: Ayo Isola, MD, assistant vice chair 2025
HISTORY OF PRESENT ILLNESS
A 50-year-old male with a past medical history of hypertension, hyperlipidemia, and type 2 diabetes mellitus presents to the emergency department with a right foot wound for 10 days. He recounts that the wound was initially uncomfortable but is now causing him extreme pain. He is also experiencing subjective fevers and chills over the past 2 days. He has been cleaning the wound and wrapping his foot daily, as he has experienced previous foot infections. He denies any recent trauma to his feet. He denies any other symptoms.
PHYSICAL EXAMINATION
 Vital signs include a blood pressure of 154/94 mmHg, heart rate of 130 beats/min, respiratory rate of 26 breaths/min, and temperature of 100.7°F (38.2°C). Physical exam shows a quarter-sized ulceration on the lateral aspect of the fifth digit on the dorsum of the right foot. There is green-blue discoloration noted proximal to the ulceration along the dorsal, lateral aspect of the fifth metatarsal. The left foot is status-post transmetatarsal amputation. There is also an amputation to the first digit on the right foot. Dorsalis pedis pulses are 2+ bilaterally. The foot motor exam is intact
Vital signs include a blood pressure of 154/94 mmHg, heart rate of 130 beats/min, respiratory rate of 26 breaths/min, and temperature of 100.7°F (38.2°C). Physical exam shows a quarter-sized ulceration on the lateral aspect of the fifth digit on the dorsum of the right foot. There is green-blue discoloration noted proximal to the ulceration along the dorsal, lateral aspect of the fifth metatarsal. The left foot is status-post transmetatarsal amputation. There is also an amputation to the first digit on the right foot. Dorsalis pedis pulses are 2+ bilaterally. The foot motor exam is intact
Fig. 1. Ulceration and cutaneous color change to the dorsal, lateral aspect of the fifth digit on the right foot
POCUS
To further assess the extent of the wound, the emergency physician performs a point-of-care ultrasound (POCUS) to the lateral aspect of the right foot using the linear probe in the musculoskeletal (MSK) preset. Within the subcutaneous tissue, numerous hyperechoic foci are present with posterior dirty shadowing (Image 1). Additionally, an anechoic layer is visualized at the suprafascial layer (Image 2).
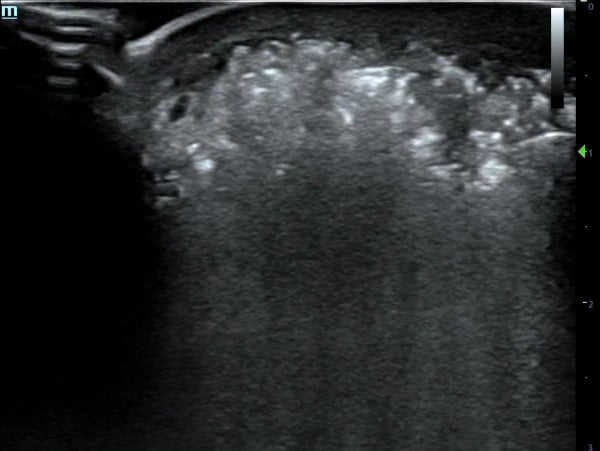
Image 1. Hyperechoic foci with posterior dirty shadowing.

Image 2. Anechoic fluid layer in the suprafascial plane (red arrow)
Video 1. Ultrasound findings upon exam
Discussion
Necrotizing fasciitis (NF) is a rare but rapidly progressive soft tissue infection characterized by widespread necrosis of the fascia and subcutaneous tissues, with an estimated annual incidence of 500-1,000 cases and prevalence of 4.0 cases per 100,000 population in the United States.1-3
On clinical examination, patients typically present with erythema, edema, warmth to palpation, and pain that is disproportionate to the physical exam, a key clinical feature.4,5 As the infection progresses, patients may experience additional signs and symptoms such as crepitus, bullae, skin discoloration, fever, and tachycardia, which can eventually lead to septic shock if not treated promptly.4,5
Due to its rapid progression and high mortality rate, ranging from 25% to 35%, early recognition of NF in the emergency department is critical, as delays often lead to poor outcomes, including limb loss and death.6,7 Risk factors include diabetes mellitus, immunosuppression, malnutrition, age > 60 years, peripheral vascular disease, renal failure, IV drug use, underlying malignancy, and obesity.1,2,5
Necrotizing fasciitis can be diagnosed through physical exam, surgical exploration, or imaging modalities such as computed tomography (CT) scan, magnetic resonance imaging (MRI), and point-of-care ultrasound (POCUS). Because NF requires early recognition and rapid decision-making, POCUS has become a valuable diagnostic tool in the emergency department, offering the advantage of immediate bedside evaluation, avoiding the potential wait time associated with CT scans and MRIs.8 Studies show that POCUS has a sensitivity ranging from 85.4% to 100% and specificity from 44.7% to 98.2%, with one study specifically noting a sensitivity of 88% and specificity of 93%.8,9 These studies based the diagnosis of necrotizing fasciitis on characteristic findings such as subcutaneous thickening, subcutaneous air, and fascial fluid collections. Fluid accumulation along the fascial plane was found to be the most sensitive finding, while subcutaneous emphysema was the most specific.9
To optimize the ultrasound settings, a linear probe should be used and set to the musculoskeletal (MSK) setting. Classic POCUS findings of NF include fascial thickening and subcutaneous tissue thickening. In gas-forming infections, the most specific finding is subcutaneous air, which appears as hyperechoic foci with posterior dirty shadowing. In contrast, in non-gas forming infections, the key finding is anechoic fluid tracking along the fascial plane, with fluid collections >4 mm considered significant.8-10
Despite the advantages of immediate evaluation, accessibility, and cost-effectiveness, POCUS is highly operator-dependent. Image quality may be limited in obese patients or patients with significant subcutaneous edema. Comparatively, CT scans prove to be a useful first-line imaging modality, as they are widely available, fast, and effective in assessing the disease, with a sensitivity of 80%.11 Similar to POCUS, CT scans show findings such as subcutaneous edema, fascial thickening, soft tissue gas, and inflammatory fat stranding.11,12 MRI is considered the imaging gold standard, as it provides high soft tissue resolution and detail, with a sensitivity of 93%.11,12 Lastly, while imaging modalities aid with diagnosis, surgical exploration remains the definitive diagnostic method.11,12
References
- Stevens DL, Bryant AE. Necrotizing soft-tissue infections. N Engl J Med. 2017;377(23):2253–2265.
- Puvanendran R, Chan Meng Huey J, Pasupathy S. Necrotizing fasciitis. Can Fam Physician. 2009;55(10):981–987.
- Misiakos EP, Bagias G, Patapis P, Sotiropoulos D, Kanavidis P, Machairas A. Current concepts in the management of necrotizing fasciitis. Front Surg. 2014;1:36.
- Goh T, Goh LG, Ang CH, Wong CH. Early diagnosis of necrotizing fasciitis. Br J Surg. 2014;101(1):e119–e125.
- Davoudian P, Flint NJ. Necrotizing fasciitis. Continuing Education in Anaesthesia Critical Care & Pain. 2012;12(5):245–250.
- Jabbour G, El-Menyar A, Peralta R, Shaikh N, Abdelrahman H, Mudali IN, Ellabib M, Al-Thani H. Pattern and predictors of mortality in necrotizing fasciitis patients in a single tertiary hospital. World J Emerg Surg. 2016;11:40.
- Sarani B, Strong M, Pascual J, Schwab CW. Necrotizing fasciitis: current concepts and review of the literature. J Am Coll Surg. 2009;208(2):279–288.
- Castleberg E, Jenson N, Dinh VA. Diagnosis of necrotizing fasciitis with bedside ultrasound: the STAFF Exam. West J Emerg Med. 2014;15(1):111-3.
- Marks A, Patel D, Sundaram T, Johnson J, Gottlieb M. Ultrasound for the diagnosis of necrotizing fasciitis: a systematic review of the literature. Am J Emerg Med. 2023;65:3135–3139
- Gan RK, Sanchez Martinez A, Abu Hasan MA, Castro Delgado R, Arcos González P. Point-of-care ultrasonography in diagnosing necrotizing fasciitis—a literature review. J Ultrasound. 2023;26(2):343–353.
- Tso DK, Singh AK. Necrotizing fasciitis of the lower extremity: imaging pearls and pitfalls. Br J Radiol. 2018;91(1088):20180093.
- Wei XK, Huo JY, Yang Q, Li J. Early diagnosis of necrotizing fasciitis: Imaging techniques and their combined application. Int Wound J. 2024;21(1):e14379.



