A leading goal for any point-of-care ultrasound (POCUS) curriculum is creating excellent, low-cost, rapid-assembly models for teaching. Associated goals include minimizing the assembly units and maximizing the number of reusable tools.
In this article, three do-it-yourself (DIY) models are described that can be used for teaching. Although initial attempts to construct the models may take up to 10 minutes, prep time for subsequent models should take approximately 5 minutes each. (Tip: A cafeteria-style tray or absorbent liner under all preparation stations is recommended to minimize cleanup.)
Vascular Access Model
This vascular access model can be repeatedly accessed with peripheral intravenous lines during a learning session.
Prep time: 5 minutes
This model is created utilizing a long cotton swab, animal balloons, water, tofu, and minimal additional tools (Figure 1).

Figure 1: Vascular access model materials
Supply list:
- Cotton swab (6-inch length)
- Animal balloons
- Cup of water
- Tofu (extra firm)
- Syringe
- Plastic container
Instructions:
- Open tofu and drain liquid.
- Place tofu on tray.
- Thread cotton swab through 1 animal balloon. Hold grip on the wooden end. Slowly extrude the balloon through the longest side of the tofu, until the balloon exits the other side. Hold the distal balloon in place and remove the cotton swab.
- Repeat step 3 to place the 2nd animal balloon.
- Utilize a syringe to remove as much air as possible from the 1st animal balloon. Fill the syringe with water and fill the animal balloon with water. Tie open end of balloon.
- Repeat step 5 with the 2nd animal balloon.
- Place in a plastic container (Figure 2).

Figure 2: Assembled vascular access model
Add a small amount of water to the tofu surface to maintain moisture, which can help reduce air artifact with repeated needle punctures. The water amount should be small and should not submerge the tofu, as that would prevent the use of the gel interface.
Utilize the linear probe and a gel interface to achieve vascular access (Figures 3 and 4).
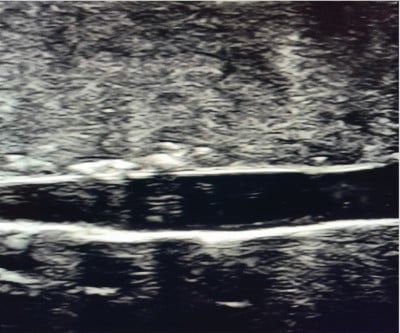
Figure 3: Ultrasound image. Vascular access model in long axis
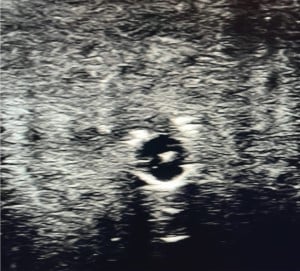
Figure 4: Ultrasound image. Vascular access model in short axis with needle tip in vein
This model is adapted from a previous vascular access model, which utilized a narrow tongue depressor for balloon extrusion and Metamucil to fill the vessels.1 The change was made from a narrow tongue depressor to a long cotton swab due to the ready availability of long cotton swabs in hospitals and from online suppliers. Narrow-width tongue depressors are less readily available than the standard type in many hospitals, and the standard type is too wide. The change from Metamucil to plain water was to help minimize ingredients and maximize efficiency. The addition of a small amount of water to the tofu surface was made due to the visualized air artifact with repeated punctures when water was not utilized.
Foreign Body Model
This foreign body (FB) model can be created for the same soft tissue learner session as the vascular model.
Prep time: <5 minutes
This model is created using tofu and FBs of various materials. The benefit of creating this model for the same session as the vascular access session is that the long cotton swab can then be broken into pieces for additional wooden and cotton FBs (Figure 5).

Figure 5: Foreign body model. FB fragments from broken cotton swab shown pre-insertion
Supply list:
- Tofu (extra firm)
- FBs (of multiple material types, such as wood, plastic, metal, and rock)
- Plastic container
Instructions:
- Open tofu and drain liquid.
- Place tofu on tray.
- Thread various FBs from the long and short sides of the tofu.
Optimal FBs are thin on the insertion aspect to minimize air introduction to the model and minimize artifacts.
Do not insert from the superior tofu aspect to avoid revealing FB locations to scanners.
Visualization is with the linear probe and a gel interface (Figure 6).

Figure 6: Ultrasound image. Foreign body model
This model is adapted from previously described FB models.1,2 The change proposed by this model is utilizing tools from the vascular model (the long cotton swabs) as foreign bodies to maximize efficient tool usage and minimize waste.
It is important to include multiple material types and sizes, as these will appear differently on ultrasound. Foreign bodies typically appear hyperechoic in relation to the surrounding tissue. Metal and glass can demonstrate reverberation artifacts and posterior acoustic shadowing to assist the scanner in locating the FBs. In contrast, other materials such as wood and plastic will demonstrate only shadowing.3,4 Sometimes, in the case of small foreign bodies, no shadowing will be evident.4
Pericardiocentesis Model
This process describes how to create a pericardiocentesis model for a cardiac learning session.
Prep time: 5 minutes, after first preparing the hearts
Preparation of the heart models: 10 minutes. The hearts are indefinitely reusable, and completing this step first minimizes preparation time for all future models.
Subsequently, preparation of the materials for the pericardiocentesis model takes approximately 5 minutes (Figure 7), with additional time determined by sink water pressure to fill the water.

Figure 7: Pericardiocentesis model materials
Heart supply list:
- Two ping pong balls
- Drill
- Stainless steel bolt and nut: two of each
Goal of heart model: An anchored ping pong ball that will sink when filled with water
Heart instructions:
- Drill 3 holes in the first ping pong ball. Two holes should be on opposite sides of the ball, and at least 2mm in diameter. The third hole should be large enough to permit tight fit of the bolt.
- Anchor creation: Spin nut onto bolt up to bolt head.
- Tighten prepared bolt into third hole of ping pong ball. Bolt should not penetrate the opposite wall of the ping pong ball.
- Repeat steps 1-3 for the second ping pong ball.
Pericardiocentesis supply list:
- Two prepared “hearts”
- Plastic food container (at least two times the height of ping pong ball)
- Larger plastic basin to hold plastic food container
- White plastic wastebasket bag
- Two snack-sized clear plastic bags (16.5cm x 8.2cm)
- Water
Pericardiocentesis model instructions:
- Place plastic food container in white plastic bag, then place both in larger plastic basin.
- Fill plastic food container with water.
- Submerge both ping pong balls in water until full.
- Submerge both snack bags in water until full.
- Place one ping pong ball in each snack bag; close the bags. Each ping pong ball simulates a heart, the surrounding water simulates the pericardial effusion, and the snack bag simulates pericardium.
- Fill the white plastic bag with additional water, then close the bag tightly and tie shut. Goal is for the bag to be filled with water, so that the level of water is mildly above the level of the plastic food container (Figure 8). The white plastic bag simulates skin.

Figure 8: Assembled pericardiocentesis model
Visualization is with the linear probe and a gel interface (Figures 9 and 10).

Figure 9: Ultrasound image. Pericardiocentesis model

Figure 10: Ultrasound image. Needle approaching pericardium in pericardiocentesis model
Each ping pong ball in the snack bag model simulates one heart with effusion.
This model is a two-heart model. The presence of two hearts helps to fill the surface area of the plastic food container, thus minimizing the motion of each heart in the water.
This model is adapted in part based on previous pericardiocentesis models.5,6
Water is utilized in this model as the pericardial effusion and soft tissue medium to minimize ingredients and reduce preparation time. Water includes no organic ingredients, and so this also permits the indefinite use of the ping pong balls for future models. The ping pong balls just need to be held in air to be emptied, then left to dry on a flat surface.
The ping pong heart model was revised to ensure it would fill and empty with water effectively without the use of a syringe. This was accomplished by increasing the number and size of the holes. The two empty holes are placed 180 degrees from each other to permit rapid water-filling and emptying via submersion and removal from the water respectively. To fill: The ball is submerged in water, with one hole on the superior aspect and one hole on the inferior aspect. Air escapes superiorly while water fills inferiorly.
An anchor was developed for the heart model, as a ping pong ball filled with water is still buoyant in water.
White plastic bags are used as the skin as these are relatively opaque, preventing scanners from seeing the heart. A partially dimmed room is utilized as this is the optimal lighting for clinical ultrasound procedures.
The benefit of the white bag being additionally filled with water is that the bag surface is thus mildly elevated above the plastic food container. This creates a taut skin surface for scanning, to better imitate pericardiocentesis conditions.
Conclusion
These three ultrasound models have been adapted from prior suggested models to optimize efficiency and minimize costs for POCUS curricula. They are currently in use for teaching at the author’s academic institution.
The author would like to thank Enrique Vega, Master of Science in Chemical Engineering, for his critical contributions to the development of the anchored ping pong ball for the heart model.
References
- Johnson G. How to Make & Practice with an Ultrasound Phantom for IVs, Lines, Abscess. YouTube. https://www.youtube.com/watch?v=I-Wqu6Tp8U4. Published August 28, 2016. Accessed August 10, 2022.
- Palmer JM, Little A, Tran QV. Cost-Effective Training Models in Point-of-Care Ultrasound for Medical Students in Emergency Medicine: An Evaluation of Current Resources. Cureus. 2022;14(4):1-7. doi:10.7759/cureus.23753
- Schlager D, Sanders AB, Wiggins D, Boren W. Ultrasound for the Detection of Foreign Bodies. Ann Emerg Med. 1991;20(2):189-191. doi:10.1016/s0196-0644(05)81220-x
- Mohammadi A, Ghasemi-Rad M, Khodabakhsh M. Non-opaque soft tissue foreign body: Sonographic findings. BMC Med Imaging. 2011;11(9):1-4. doi:10.1186/1471-2342-11-9
- Campo dell’Orto M, Hempel D, Starzetz A, et al. Assessment of a Low-Cost Ultrasound Pericardiocentesis Model. Emerg Med Int. 2013;2013:1-7. doi:10.1155/2013/376415
- Kalivoda EJ, Sullivan A, Bunting L. A Cost-Effective, Rapidly Constructed Simulation Model for Ultrasound-Guided Pericardiocentesis Procedural Training. J Emerg Med. 2019;56(1):74-79. doi:10.1016/j.jemermed.2018.09.010



