A 20-year-old female with no remarkable past medical history presented to the ED with a chief concern of 3 days of dark urine. The patient reported previously noted dark urine a few weeks prior to this presentation, with full spontaneous resolution.
In both episodes the patient had not experienced dysuria, vaginal discharge, urinary urgency or frequency, and these episodes occurred outside the patient's normal menstrual cycle. The patient also endorsed an approximately 1-week history of concomitant subjective warmth, fatigue, dry cough, tension-type headaches (similar to prior headaches and without concerning features), xerostomia, and reduced oral fluid intake. Further, the patient reported 2 episodes of urticaria each lasting less than 1 hour occurring in the 3 days prior to her ED visit. The first episode was noted on her bilateral upper extremities while the second presented over her bilateral lower extremities. Both episodes resolved spontaneously and the patient denied any use of novel cleansing products, fabrics, or awareness of other potential exposures.
On ED arrival, the patient's vital signs were recorded as a pulse 150, blood pressure 122/71, temperature 37.5°C, and oxygen saturation 99% on room air. Overall, the patient was well-appearing and the physical examination was unremarkable apart from the presence of dry mucous membranes without notable hepatosplenomegaly, lymphadenopathy, or other concerning findings. Urinalysis was notable for the presence of amber colored urine with 1+ protein, 2+ urobilinogen, 41 white blood cells per high powered field, and many bacteria. The sample was contaminated by 58 squamous epithelial cells, positive for nitrites, and negative for red blood cells (RBCs). Complete metabolic panel was remarkable for a transaminitis with alanine aminotransferase (ALT) elevated to 169 and aspartate aminotransferase (AST) elevated to 185, alkaline phosphatase (ALP) elevated to 129, and direct bilirubin elevated to 0.4 with a total bilirubin of 1.2. Complete blood count demonstrated a normocytic anemia with hemoglobin (Hb) 8.9, hematocrit 24, RBC count 2.54, and mean corpuscular volume (MCV) 93. White blood cell count was within normal limits at 8.3k/mm3 and absolute lymphocyte count elevated to 3,840/mm3 cells. Electrocardiography revealed sinus tachycardia with ventricular rate 124.
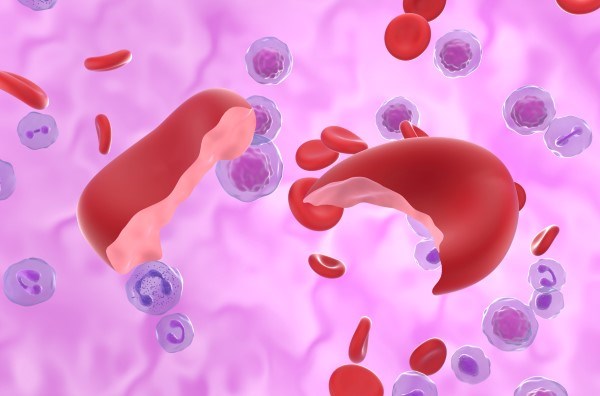
With no history of anemia, liver disease, and in the absence of hematuria, these results were concerning for an active hemolytic process potentially related to an underlying infection. Further testing revealed elevated lactate dehydrogenase (LDH) 1,108 U/L, haptoglobin <10 mg/dL, and a reticulocyte count 5.4% and 198.4 k/mm3 cells. Peripheral blood smear was positive for polychromasia, target cells, and RBC agglutination. Epstein-Barr heterophile antibody testing was positive and additional viral testing for influenza A/B, COVID-19, and respiratory syncytial virus was otherwise negative. Ferritin was elevated to 192 ng/mL—however iron level, iron percent saturation, total iron binding capacity, and transferrin were all within normal limits. A direct antiglobulin test was performed and was positive for complement C3 and negative for immunoglobulin G (IgG). Cold agglutinin titer testing returned positive at 1:128. Findings consistent with a diagnosis of cold agglutinin autoimmune hemolytic anemia (AIHA), believed secondary to infectious mononucleosis.
In accordance with hematology recommendations, the patient was covered in warmed blankets with special care to acral areas. A repeat Hb was obtained decreasing to 7.8 from 8.9 g/dL. The patient was subsequently admitted for observation to the hospitalist service. Transfusion was not indicated during the admission as the patient’s Hb levels ranged from a low of 7.2 g/dL before uptrending to 8.6 g/dL prior to discharge. Further testing demonstrated broad reactivity of the patient’s plasma with cord blood cells and less so with her own RBCs at 1-6°C and weak reactivity at ambient room temperatures. Due to continued improvement the patient was ultimately discharged in stable and improved condition on hospital day 3.
Discussion
Cold agglutinin syndrome is an AIHA mediated by cold agglutinin, typically monoclonal, proteins. Primarily, these proteins consist of IgM autoantibodies, although IgA and IgG proteins have been reported in the literature.1-3 These autoantibodies are invariably directed against specific RBC surface antigens of the I and i types. Binding across multiple antigen binding sites on each autoantibody leads to the agglutination characteristic of the disease process. Anti-I antibodies are usually associated with primary cold agglutinin disease and Mycoplasma infection whereas anti-i antibodies are more commonly associated with Epstein-Barr virus (EBV) infections.4 As i antigens are vastly more prevalent on infantile RBCs, the patient’s plasma being more strongly reactive with cord blood than with her own RBCs is further evidence of the diagnosis.
This pathology is termed "cold" as the agglutinin proteins bind to their target antigens between 0-4°C and are most active between 3-4°C.5 If the patient's blood is cooled, often occurring organically in acral regions of the body, cold agglutinin will bind to the RBCs and the resultant agglutination may precipitate circulatory symptoms such as Raynaud-like phenomenon or acrocyanosis. Additionally, complement-mediated hemolysis results as the now bound IgM recruits complement C1 leading to classical pathway activation and ultimately to macrophage phagocytosis.6 This hemolysis is principally extravascular and occurs in hepatic Kupffer cells.4
While most cases comprise a primary autoimmune process and are more properly termed cold agglutinin disease (CAD), cold agglutinin AIHA may complicate other disease processes such as EBV infection, as occurred in this case, as well as Mycoplasma pneumoniae pneumonia and certain lymphomas, and in such cases is then generally referred to as secondary cold agglutinin syndrome (CAS).6,7 Mycoplasma or primary atypical pneumonia has been identified as the likely underlying cause in 8% of AIHA cases and EBV rarer still and implicated in ~1% of cases, although the overall frequency of clinically significant hemolysis in both of these disease processes is unknown.8 Believed quite rare overall, CAD has an incidence of 1/million, though this is likely an underestimation due to lack of clinical recognition.9
Diagnosis of CAD/CAS should begin with testing including a CBC with peripheral blood smear, LDH, haptoglobin, and indirect bilirubin. A direct antiglobulin (Coombs) test should be performed if workup is concerning for AIHA. Finally, a cold agglutinin titer should be obtained. Should testing concomitantly demonstrate evidence of hemolysis with a positive Coombs test and cold agglutinin titer >1:64 (higher number indicating greater presence of autoantibodies) at 4°C, the diagnosis is made.1
Generally, secondary CAS does not warrant specific treatment beyond supportive care and management of the underlying disease process as in this case.7 Supportive care should most prominently consist of cold temperature avoidance to reduce further agglutination and hemolysis. Should the patient’s Hb levels enter a transfusable range, this may be safely performed. More emergent and temporizing measures such as plasmapheresis, intravenous immunoglobulin (IVIG), and complement inhibitors such as eculizumab or sutimlimab may be warranted in individuals experiencing symptomatic or severe anemia.7,10 In contrast, glucocorticoids are ineffective as they fail to inhibit IgM antibody production and should not be administered.11 Should the EM physician suspect primary CAD, referral to, or consultation with, hematology is advised for consideration of management with rituximab-bendamustine or rituximab monotherapy.12
Take-Home Points
Cold agglutinin syndrome (CAS) represents an autoimmune process resulting in complement-dependent hemolytic anemia usually mediated by IgM autoantibodies known to complicate various infections and malignancies. Although most cases secondary to infection are mild, transient, and resolve with the underlying infection, ~1/3 of patients develop anemia with hemoglobin levels <8 g/dL. In these instances, treatment beyond supportive measures such as cold avoidance, active rewarming, blood transfusion, and the initiation of additional pharmacotherapies may be warranted.
As infectious mononucleosis is a common diagnosis made in the emergency department (ED) setting and CAS, a relatively under discussed complication, it is quite likely that many cases go undiagnosed. Though uncommonly requiring interventions beyond supportive care, it is nonetheless important for the EM physician to be familiar with this potentiality given an increased risk of morbidity and mortality in those diagnosed with EBV infectious mononucleosis. A high index of suspicion is indicated when patients testing positive for EBV present with associated findings such as acrocyanosis, dark urine, fatigue, pallor, or jaundice, and otherwise unexplained anemia as further management may be indicated.
References:
- Berentsen S. How I manage patients with cold agglutinin disease. Br J Haematol. 2018;181(3):320-330.
- Pereira A, Mazzara R, Escoda L, Alcorta I, Nomdedeu B, Roelcke D. Anti-Sa cold agglutinin of IgA class requiring plasma-exchange therapy as early manifestation of multiple myeloma. Ann Hematol. 1993;66(6):315-318.
- Silberstein LE, Berkman EM, Schreiber AD. Cold Hemagglutinin Disease Associated with IgG Cold-Reactive Antibody. Ann Intern Med. 1987;106(2):238.
- Zilow G, Kirschfink M, Roelcke D. Red Cell Destruction in Cold Agglutinin Disease. Transfus Med Hemother. 1994;21(6):410-415.
- Berentsen S. Cold agglutinin disease. Hematology Am Soc Hematol Educ Program. 2016;2016(1):226-231.
- Berentsen S, Randen U, Tjønnfjord GE. Cold agglutinin-mediated autoimmune hemolytic anemia. Hematol Oncol Clin North Am. 2015;29(3):455-471.
- Jäger U, Barcellini W, Broome CM, et al. Diagnosis and treatment of autoimmune hemolytic anemia in adults: Recommendations from the First International Consensus Meeting. Blood Rev. 2020;41:100648.
- Berentsen S, Tjønnfjord GE. Diagnosis and treatment of cold agglutinin mediated autoimmune hemolytic anemia. Blood Rev. 2012;26(3):107-115.
- Berentsen S, Ulvestad E, Langholm R, et al. Primary chronic cold agglutinin disease: A population based clinical study of 86 patients. Haematologica. 2006;91(4):460-466.
- Röth A, Barcellini W, D'Sa S, et al. Sutimlimab in Cold Agglutinin Disease. N Engl J Med. 2021;384(14):1323-1334.
- Berentsen S, Barcellini W. Autoimmune Hemolytic Anemias. N Engl J Med. 2021;385(15):1407-1419.
- Berentsen S. How I treat cold agglutinin disease. Blood. 2021;137(10):1295-1303.