The Lisfranc joint complex, also known as the tarsometatarsal (TMT) joint complex, is essential for maintaining the arch of the midfoot.1 The TMT joint complex functions as a pivotal joint for midfoot function and stability, particularly with weight-bearing activities.
The main osseous architecture comprising the TMT joint complex is the articulation in the midfoot between all three cuneiforms, the cuboid, and the metatarsal bones.
Lisfranc injuries are typically categorized into high-energy and low-energy mechanisms. High-energy mechanisms involve significant axial loading or rotational forces that cause either ligamentous injury or fracture dislocation at the TMT joint. Low-energy mechanisms are most commonly caused by axial loading or twisting while the foot is planted.2 Direct trauma to the midfoot can also result in Lisfranc injuries.3
Injuries to the Lisfranc complex may be misdiagnosed or go untreated, which is associated with substantial morbidity due to its intricate role in biomechanics and maintaining the arch of the foot. When the joint is injured, the injury results in abnormal weight distribution and biomechanical changes in the foot arch.3 The location and severity of a Lisfranc injury will determine if surgery is recommended.1
Case Presentation
A 49-year-old male patient presents to the emergency department due to 1 week of left foot pain and swelling. The patient suffered from a cardiac arrest following a witnessed syncopal collapse while carrying groceries. Since he was discharged from the hospital, despite a negative foot X-ray completed as an inpatient, he has continued to have difficulty ambulating due to significant pain, and noticed progressive bruising of the foot. Physical exam was notable for midfoot and forefoot swelling, significant ecchymosis of the plantar midfoot and lateral foot, and dorsal and plantar midfoot tenderness to palpation overlying the Lisfranc complex. Metatarsal squeeze test was positive. Remainder of the left lower extremity exam was unremarkable.
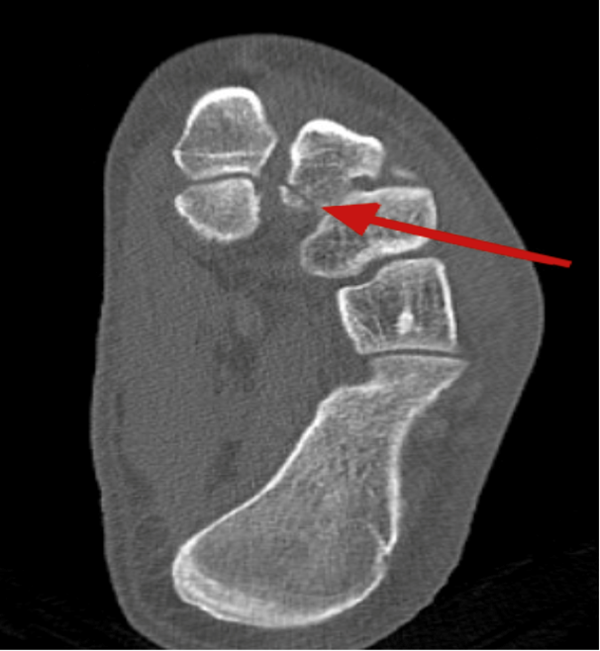
Recent AICD placement precluded the patient from obtaining an outpatient MRI. A CT scan of the foot was performed in the ED, which demonstrated an acute non-displaced intra-articular fracture at the insertion of the Lisfranc ligament at the base of the 2nd metatarsal with otherwise normal tarsal-metatarsal alignment.
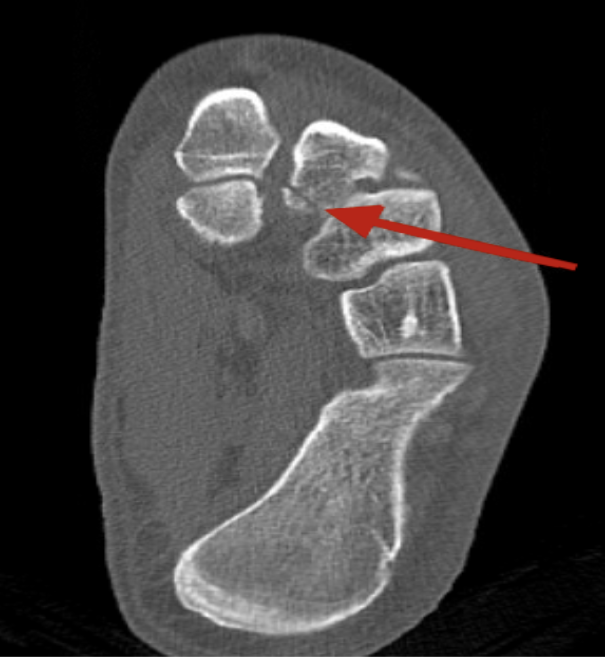
Figure 1: Initial foot X-ray read as normal, cortical irregularity seen at base of 2nd metatarsal

Figure 2: CT of left foot demonstrating fracture at base of 2nd metatarsal
Clinical Examination Findings
The clinical exam findings in patients with Lisfranc injuries vary based on the type and severity of the injury. There will likely be pain and tenderness overlying the TMT joint complex, swelling of the midfoot region, or plantar ecchymosis.2 Stress testing for instability of the TMT joint may show dorsal subluxation suggestive of instability.4 Neurologic deficits or compromised blood flow due to compartment syndrome are relatively rare but can occur, and may accompany severe dislocations or fractures.
X-rays of the foot may be unremarkable, demonstrate subtle diastasis at the base of the 1st and 2nd metatarsals, or reveal a fracture such as a “fleck sign” at the base of the 1st or 2nd metatarsal.5 CT or MRI may help to confirm diagnosis, with MRI being a preferred modality to evaluate Lisfranc joint complex in addition to bony structures.6
Discussion and Management
Alternative diagnoses that may be considered when evaluating for Lisfranc injuries include midfoot and metatarsal shaft fractures, soft tissue injury, and vascular etiologies. However, XR imaging and vascular studies will show different patterns of injury and pathology that are not typically seen with Lisfranc injuries.
Management of Lisfranc injuries may be conservative or surgical based on the severity of the injury. Non-operative management may be considered for non-displaced injuries or those with minimal disruption of the TMT joint complex.2 For patients evaluated in the ED with concern for Lisfranc injury, it is reasonable to immobilize with a boot or short leg splint/cast, encourage non-weight-bearing status, and provide crutches to assist ambulation and mitigate risk of worsening injury. It is imperative for patients to follow up closely as an outpatient with a sports medicine provider, podiatrist, or orthopedic foot/ankle specialist within 1-2 weeks for continued management to ensure that there is no injury progression or in case surgical fixation is indicated.
Early diagnosis and appropriate management favor a positive outcome.6 Surgical intervention generally leads to better functional outcomes in cases of displaced fractures or joint instability. However, this can come with long-term complications such as arthritis, stiffness, and post-traumatic deformities such as midfoot arthritis and arch collapse.7,8
Case Resolution
At discharge, the patient was provided with a walking boot and advised to limit weight bearing on the affected extremity with use of cane (unfortunately for the patient, broken ribs suffered from CPR made use of crutches difficult). He was able to follow up with a podiatrist the following week, and treatment options including surgical fixation and non-weight bearing in a short leg cast were suggested, but the patient declined.
References
- Mascio A, Greco T, Maccauro G, Perisano C. (2022). Lisfranc complex injuries management and treatment: current knowledge. International Journal of Physiology, Pathophysiology and Pharmacology, 14(3), 161–170.
- Grewal US, Onubogu K, Southgate C, Dhinsa BS. (2020). Lisfranc injury: A review and simplified treatment algorithm. Foot (Edinburgh, Scotland), 45, 101719.
- Buchanan BK, Donnally III CJ. (2025). Lisfranc Dislocation. In StatPearls. StatPearls Publishing.
- Yan A, Chen SR, Ma X, Shi Z, Hogan M. (2021). Updates on Lisfranc Complex Injuries. Foot & Ankle Orthopaedics, 6(1), 2473011420982275.
- Taylor KS, Achar SA. (Eds.). (2020). The 5-minute sports medicine consult (3rd edition). Wolters Kluwer.
- Mulier T, De Haan J, Vriesendorp P, Reynders P. The Treatment of Lisfranc Injuries: Review of Current Literature. Eur J Trauma and Emerg Surg. 2010;36(3):206–216.
- Eiff MP, Hatch R. (2021). Fracture management for primary care and emergency medicine. (Fourth edition). Elsevier.
- Philbin T, Rosenberg G, Sferra JJ. (2003). Complications of missed or untreated Lisfranc injuries. Foot and Ankle Clinics, 8(1), 61–71.