ARTICLE: Polymeris AA, Karwacki GM, Siepen BM, et al. for the TICH-NOAC Investigators. Tranexamic Acid for Intracerebral Hemorrhage in Patients on Non-Vitamin K Antagonist Oral Anticoagulants (TICH-NOAC): A Multicenter, Randomized, Placebo-Controlled, Phase 2 Trial. Stroke. 2023;54(9):2223-2234.
OBJECTIVE
To assess the efficacy and safety of Tranexamic Acid (TXA) in Non-Vitamin K Antagonist Oral Anticoagulants (NOAC)-associated intracerebral hemorrhage (ICH)
BACKGROUND
Intracerebral hemorrhage (ICH) is associated with high morbidity and mortality,1 and is further complicated in the setting of oral anticoagulation, which increases the risk of hematoma expansion (HE).2 Novel, non-vitamin K antagonist oral anticoagulants (NOACs) are the pillar of oral anticoagulation and have greatly replaced vitamin K antagonists in current practice.3 As a result, NOAC-associated ICH has also increased, leading to higher rates of HE, in-hospital mortality and disability.4-6 No evidence-based treatment currently exists to help achieve hemostasis in NOAC-associated ICH.7,8 While reversal agents exist for specific NOACs (eg, andexanet alfa for factor Xa inhibitors like apixaban or rivaroxaban and idarucizumab for direct thrombin inhibitors like dabigatran), evidence is lacking on whether they are superior to current standards of care.9,10 Current guidelines recommend using these NOAC-specific reversal agents combined with 4-factor prothrombin complex concentrate (4fPCC).7,8,11
Tranexamic acid (TXA) is an antifibrinolytic drug that does not affect coagulation factors such as thrombin or factor Xa. Instead, it blocks endogenous fibrinolysis, delaying clot degradation and stabilizing fibrin clot formation.12 TXA was recently studied in non-NOAC-associated ICH in the Tranexamic Acid for Hyperacute Primary Intracerebral Hemorrhage (TICH-2) trial, which ultimately found no significant difference in functional status 90 days after ICH between those who received TXA and those who received a placebo, though a reduction in early deaths and serious adverse effects were found in the TXA group.13 TXA has also been shown to have potential in reducing HE in certain populations with spontaneous ICH.14,15 This trial examines the effects of TXA on HE in NOAC-associated ICH compared to current standard medical care.
DESIGN
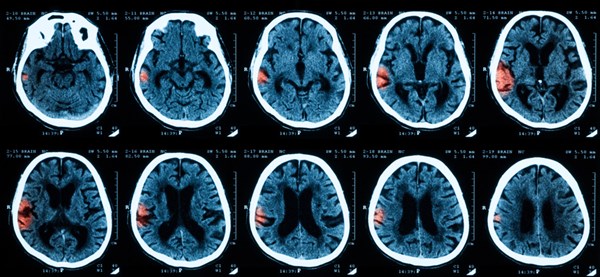
Double-blind, randomized, placebo-controlled, investigator-led phase 2 trial at 6 stroke centers in Switzerland from December 2016 to September 2021. All participants were administered either IV TXA as an initial 1 g loading dose in 100 mL normal saline infused over 10 minutes and followed by another 1 g in 250 mL normal saline infused over 8 hours or placebo with identical administration procedure. The rest of the patient's care was left to standard medical practice, which included blood pressure management and use of other hemostatic agents at the discretion of the treatment team. Baseline CT scans were done as part of routine care before randomization. A follow-up CT scan was done after 24±3 hours to assess HE.
INCLUSION CRITERIA
- Adults with acute non-traumatic intracranial hemorrhage (ICH) that could be randomized within 12 hours of symptom-onset and were taking any NOAC (apixaban ≥ 2.5 mg, dabigatran ≥ 110 mg, edoxaban ≥ 30 mg, or rivaroxaban ≥ 10 mg) with known last intake within 48 hours or proven persistent NOAC activity using NOAC-specific coagulation assays.
EXCLUSION CRITERIA
- Severe pre-existing disability (modified Rankin Scale [mRS] score >4)
- GCS < 5
- Prior treatment with vitamin K antagonists
- ICH known or suspected to be secondary to trauma, vascular malformation, tumor, or other underlying structural abnormality
- Pregnancy
- Planned neurosurgical hematoma evacuation within 24 hours
- Pulmonary embolism or deep vein thrombosis within preceding 2 weeks
Of note, concurrent use of other hemostatic agents (eg, idarucizumab, andexant alfa, and 4-factor PCC) was not an exclusion criterion.
PRIMARY OUTCOME
Presence of HE on follow-up imaging at 24±3 hours, defined as intracerebral hematoma volume increase by at least 33% or 6mL from baseline
SECONDARY OUTCOMES
- Symptomatic HE, defined as hematoma expansion with neurological deterioration (worsening of NIHSS score by at least 4 points or GCS score by at least 2 points) or death within 7 days
- Absolute hematoma volume change by 24±3 hours
- Ordinal mRS score, mRS score 0 to 4, and mRS score 0 to 3 at 90 days
- In-hospital death
- Death within 90 days
- Major thromboembolic events (ischemic stroke, myocardial infarction, or deep vein thrombosis/pulmonary embolism) within 90 days
- Neurosurgical intervention up to day 2
KEY RESULTS
- A total of 67 patients were enrolled between December 12, 2016, and September 30, 2021. Unfortunately, the trial was discontinued early due to exhausted funding (intended to get 109 patients enrolled).
- 4 patients were withdrawn immediately after randomization
- 32 assigned to TXA and 31 to placebo
- 2 died before follow-up imaging (1 in TXA group, 1 in placebo group)
- 59 received treatment per protocol (29 in TXA group, 30 in placebo group)
- Follow-up imaging done at median of 24 hours after baseline imaging (25.9 hours after symptom onset)
- Median age was 82 years, 40% were women
- All patients were taking direct factor Xa inhibitors (apixaban, edoxaban, rivaroxaban); none were taking direct thrombin inhibitors (dabigatran)
- The most common NOAC taken by patients was rivaroxaban (78% of participants)
- Atrial fibrillation was the leading indication for anticoagulation (87% of participants)
- No participants received NOAC-specific reversal agents while 41 (65%) concomitantly received 4fPC
Primary Outcome
In total, 41% (26/63) of study patients had HE, 38% (12/32) in the TXA group and 45% (14/31) in the placebo group (adjusted OR 0.63 [95% Cl, 0.22-1.82], p=0.4). These results were not statistically significant
Secondary Outcomes
- None of the prespecified secondary outcomes differed between treatment arms
- There were 9.5% (6/63) of patients who had major thromboembolic event within 90 days, 12.5% (4/32) of those who received TXA and 6.5% (2/31) of those who received placebo (OR 1.86 [95% Cl, 0.37-9.50], p=0.45)
- No difference was noted between the arms in terms of recorded seizures within 90 days, 19% (6/32) in the TXA group and 13% (4/31) in the placebo group (adjusted OR 1.62 [0.22-1.89], p=0.49)
- No difference was noted in rate of participants with any serious adverse events (including major thromboembolic events, seizures, and death) up to 90 days, and any serious adverse events up to day 7: up to 75% (24/32) in the TXA group and 65% (20/31) in the placebo group (adjusted OR 1.43 [0.45-4.47], p=0.54)
- Signal for interaction with onset-to-treatment time of ≤6 hours (p=0.024) and ANNEXa-I eligibility (ongoing randomized control trial investigating andexanet alfa in patients with factor Xa-inhibitor-associated ICH, p=0.025)
LIMITATIONS
- Failure to reach target sample size resulting in an underpowered sample size and subgroup analyses with wide confidence intervals
- Premature discontinuation of TICH-NOAC due to lack of funding and the negative impact of the COVID-19 pandemic on research activities, which slowed participant recruitment and prevented expansion of the trial to international sites
EM TAKE-AWAYS
In this underpowered RCT, no evidence was found that TXA limits HE nor that it improves clinical outcomes by 90 days in NOAC-associated ICH. That being said, there were no major safety concerns noted in the use of TXA and there was a signal that it may be beneficial for preventing HE in select patients, particularly those treated within 6 hours of ICH onset.
REFERENCES
- Poon MT, Fonville AF, Al-Shahi Salman R. Long-term prognosis after intra-cerebral haemorrhage: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2014;85:660–667.
- Seiffge DJ, Goeldlin MB, Tatlisumak T, Lyrer P, Fischer U, Engelter ST, Werring DJ. Meta-analysis of haematoma volume, haematoma expansion and mortality in intracerebral haemorrhage associated with oral anticoagulant use. J Neurol. 2019;266:3126–3135.
- Hald SM, Möller S, García Rodríguez LA, et al. Trends in incidence of intracerebral hemorrhage and association with antithrombotic drug use in Denmark, 2005-2018. JAMA Netw Open. 2021;4(5):e218380.
- Wilson D, Seiffge DJ, Traenka C, et al., for the CRO-MIS-2 Collaborators. Outcome of intracerebral hemorrhage associated with different oral anticoagulants. Neurology. 2017;88(18):1693–1700.
- Tsivgoulis G, Wilson D, Katsanos AH, et al. Neuroimaging and clinical outcomes of oral anticoagulant-associated intracerebral hemorrhage. Ann Neurol. 2018;84(5):694–704.
- Inohara T, Xian Y, Liang L, et al. Association of intracerebral hemorrhage among patients taking non-vitamin K antagonist vs vitamin K antagonist oral anticoagulants with in-hospital mortality. JAMA. 2018;319(5):463–473.
- Christensen H, Cordonnier C, Kõrv J, et al. European Stroke Organisation guideline on reversal of oral anti-coagulants in acute intracerebral haemorrhage. Eur Stroke J. 2019;4:294–306.
- Greenberg SM, Ziai WC, Cordonnier C, et al., for the American Heart Association/American Stroke Association. 2022 guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022;53:e282–e361.
- Pollack CV, Reilly PA, van Ryn J, et al. Idarucizumab for dabigatran reversal — full cohort analysis. N Engl J Med. 2017;377:431–441.
- Connolly SJ, Crowther M, Eikelboom JW, et al. Full study report of andexanet alfa for bleeding associated with factor Xa inhibitors. N Engl J Med. 2019;380:1326–1335.
- Gómez-Outes A, Alcubilla P, Calvo-Rojas G, Terleira-Fernández AI, Suárez-Gea ML, Lecumberri R, Vargas-Castrillón E. Meta-analysis of reversal agents for severe bleeding associated with direct oral anticoagulants. J Am Coll Cardiol. 2021; 77:2987–3001.
- Levy JH. Antifibrinolytic therapy: new data and new concepts. Lancet. 2010;376:3–4.
- Sprigg N, Flaherty K, Appleton JP, et al., for the TICH-2 Investigators. Tranexamic Acid for Hyperacute Primary Intra-cerebral Haemorrhage (TICH-2): an international randomised, placebo-controlled, phase 3 superiority trial. Lancet. 2018; 391:2107–2115.
- Guo Y, Guo XM, Li RL, et al. Tranexamic acid for acute spontaneous intracerebral hemorrhage: a meta-analysis of randomized controlled trials. Front Neurol. 2021;12:761185.
- Meretoja A, Yassi N, Wu TY, et al. Tranexamic acid in patients with intra-cerebral haemorrhage (STOP-AUST): a multicentre, randomised, placebo-controlled, phase 2 trial. Lancet Neurol. 2020;19:980–987.