A 22-month-old male presented to the pediatric ED for approximately 6 weeks of daily fever with temperatures greater than 101°F both oral and axillary, decreased appetite, increasing fatigue, and new-onset right upper quadrant pain.
When the fever first began, he was seen at an urgent care center and diagnosed with acute otitis media. 1 week later, he was again seen at urgent care for continued fevers and a swollen toe. He was diagnosed with cellulitis and prescribed cefdinir, but the fever persisted despite antibiotics. He was then taken twice to the emergency department, where he was diagnosed with enterovirus/rhinovirus and treated with ceftriaxone for leukocytosis noted on CBC.
On this presentation, the family was concerned for his persistent fever and nasal congestion but no other active symptoms. Social history was negative for travel. He had contact with dogs and cats at home. Review of systems was positive for fevers, right upper quadrant abdominal pain, decreased appetite, headache, and fatigue. There was no report of cough, hemoptysis, weight loss, night sweats, joint pain or swelling, rashes, swollen glands, or mucosal changes. On exam, vitals were normal and he was afebrile at 99F. He had cervical lymphadenopathy with a right-sided 2 cm soft mobile lymph node. Labs were significant for leukocytosis, elevated ESR and CRP, normal uric acid, and mildly elevated LDH. Titers for zoonoses and viral infections like EBV, typhus, Bartonella, and CMV were sent and remained pending while in the ED. Given lab results and clinical history, infectious disease was consulted due to this presumed fever of unknown origin. ID recommended inpatient admission and an abdominal ultrasound given cat exposure and risk for disseminated cat-scratch disease. After admission, the ultrasound showed multiple cystic lesions in the liver and spleen, consistent with disseminated cat-scratch disease. (Figures 1 and 2)
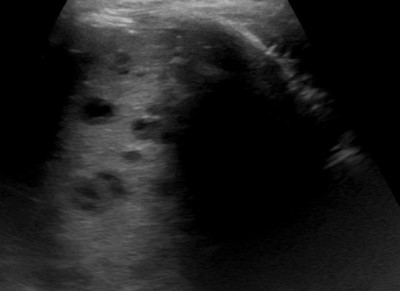
Figure 1 (above)
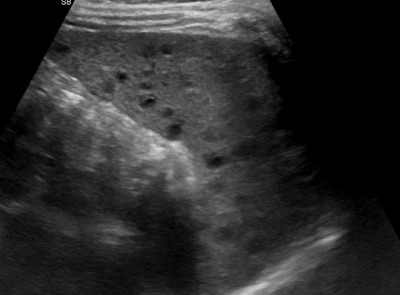
Figure 2 (above)
Discussion
Bartonellosis is a zoonotic infectious disease caused by Bartonella henselae, a gram-negative bacterium. It typically presents as benign cat-scratch disease (CSD) in about 90% of cases, predominantly in the summer-autumn months.1The pediatric incidence of CSD is approximately 4 per 100,000, with the highest incidence at ages 5-9 years.2
Cat-scratch disease typically presents after a bite or scratch from a cat, more commonly a kitten, resulting in localized painful lymphadenopathy, fever, malaise, rash, and headache. Although kittens are the natural carriers of bartonella, it should be said that it is also associated with dogs since the transition occurs primarily through flea bites.1
Often cat-scratch disease goes undiagnosed and resolves spontaneously without antibiotic treatment. However, approximately 5-25% of CSD cases are atypical or disseminated, where the infection has spread from the site of inoculation to other visceral organs such as the heart, eyes, liver, spleen, or brain.
A CSD diagnosis is typically done through a combination of clinical findings, historical exposure to cats, and serologic testing. Atypical CSD can present with nonspecific symptoms such as abdominal pain, weight loss, headache, and fever of unknown origin. It is the investigation of fever of unknown origin that characteristically leads to the diagnosis of atypical CSD, as in our patient.
Behind typhoid fever and urinary tract infections, CSD is the third most common cause of FUO and should be high on the differential whenever a child with prolonged fever presents to the emergency department.3 Hepatosplenic CSD, a subset of atypical CSD, more commonly occurs with FUO and other systemic symptoms such as abdominal pain and weight loss. The evaluation of patients suspected of having disseminated CSD should include CBC, inflammatory markers such as ESR and CRP, and serologic titers both IgG and IgM.
Because of the high prevalence of CSD in association with FUO, abdominal imaging is essential in these patients. Almost 70% of patients with hepatosplenic CSD will have microabscesses in their spleen and liver.4 These abscesses typically present as hypoechoic lesions on ultrasound and histologically represent necrotizing granulomas. Most recently it has been suggested that hepatosplenic involvement may be associated with even typical CSD, since one study has found a hepatosplenic compromise in both cases of typical and atypical CSD.2 Nevertheless, management of patients with hepatosplenic CSD and other forms of atypical CSD has been somewhat controversial, since antibiotic therapy for even typical CSD is not generally indicated but is used for shortening the duration of symptoms. Most children who are hospitalized due to disseminated CSD receive antibiotic therapy for symptomatic management as well as to prevent further complications, especially in cases of aseptic meningitis, neuroretinitis, and culture-negative endocarditis.
|
Typical CSD |
Atypical CSD |
|
Regional tender lymphadenopathy |
Hepatosplenic abscesses |
|
Vesicular lesion at site of inoculation |
Neuroretinitis/ Parinaud oculoglandular syndrome |
|
|
Endocarditis |
|
|
Encephalitis |
Management of Atypical CSD
There is no consensus on the treatment of atypical CSD. Various case series and reports have proposed a mixture of regimens that include azithromycin, rifampin, gentamicin, trimethoprim/sulfamethoxazole, and broad spectrum cephalosporins. However, no in vivo RCTs have been conducted to compare efficacy. Only one in vivo RCT has been done to evaluate the effect of azithromycin on CSD. That trial found a significant reduction in lymph node size in the treatment group.5 Therefore, treatment is individualized and based largely on symptom severity. Perhaps the most utilized regimen for hepatosplenic CSD is a 14-day course of rifampin, either alone or in combination therapy. 4 This regimen has been shown to be highly effective in most immunocompetent patients with almost none of those patients developing persistent CSD. Other antibiotic regimens include azithromycin alone for 14 days, gentamicin in combination with TMP-SMX, and rifampin for up to 4 weeks. The precise treatment of hepatosplenic CSD remains unclear, however, the literature recommends treatment for all patients diagnosed. The clinical response in a patient who is immunocompromised compared to immunocompetent is dramatically improved when treated with antibiotics.
Case Conclusion
The patient was started on azithromycin and rifampin for 14 days based on ID recommendations. He was discharged home with ID outpatient follow-up. Several days after discharge, the patient’s serologic titers came back positive with IgG 1:1024 and IgM 1:128. The family, when called, said his fevers had resolved and he was back to his normal activity level.
Atypical cat-scratch disease can manifest in a variety of ways, most notably hepatosplenic disease in both the immunocompetent and immunocompromised child. Recognizing that this disease is one of the top causes of fever of unknown origin is important in the diagnosis and management of pediatric patients. Undiagnosed cat-scratch disease can have high morbidity. Therefore, it is important for emergency physicians to correlate a good history and physical examination, as well as appropriate laboratory and imaging studies, in order to appropriately treat these patients.
References
- Lemos AP, Domingues R, Gouveia C, de Sousa R, Brito MJ. Atypical bartonellosis in children: What do we know? J Paediatr Child Health. 2021;57(5):653-658.
- Sandoval AC, Reyes FT, Prado MA, Peña AL, Viviani TN. Cat-scratch Disease in the Pediatric Population: 6 Years of Evaluation and Follow-up in a Public Hospital in Chile. Pediatr Infect Dis J. 2020 Oct;39(10):889-893.
- Finkelstein JA, Christiansen CL, Platt R. Fever in pediatric primary care: occurrence, management, and outcomes. Pediatrics. 2000;105(1 Pt 3):260-6.
- Florin TA, Zaoutis TE, Zaoutis LB. Beyond cat scratch disease: widening spectrum of Bartonella henselaeinfection. Pediatrics. 2008 May;121(5):e1413-25.
- Bass JW, Freitas BC, Freitas AD, et al. Prospective randomized double blind placebo-controlled evaluation of azithromycin for treatment of cat-scratch disease. Pediatr Infect Dis J. 1998 Jun;17(6):447-52.



