POCUS is a key diagnostic tool that can allow emergency physicians to diagnose a range of injuries. This case highlights the utility of bedside point-of-care ultrasound in offering a specific and sensitive diagnosis in a case of penile fracture.
This paper was edited by:
HISTORY OF PRESENT ILLNESS
A 45-year-old man with a past medical history of psoriasis and asthma presents to the ED at 2 AM reporting penile pain that occurred during sexual intercourse prior to arrival. He describes hearing a pop followed by sudden detumescence and swelling of his penis. Review of systems was negative for difficulty urinating, dysuria, hematuria, blood at meatus, penile discharge, or testicular pain.
PHYSICAL EXAMINATION
Vital signs including a blood pressure of 142/96, pulse 84 beats/minute, respiratory rate 19 breaths/min, oxygen saturation of 99%, and a temperature 98°F. Genitourinary examination reveals a left pointing curvature of the penis, fusiform swelling with an Aubergine sign described as "eggplant deformity" (Figure 1). The testicular exam is normal including an intact cremasteric reflex. No penile tenderness or blood at urethral meatus is noted. The patient endorses being able to urinate without any complications.

Figure 1. Left-pointing curvature of the penis with fusiform swelling, Aubergine sign described as "eggplant deformity"
POCUS
Due to concern for a penile fracture, the emergency physician performed a point-of-care ultrasound (POCUS) of the penile shaft in sagittal and transverse views using the 5 mHz – 12 mHz linear probe in the musculoskeletal preset to evaluate the tunica albuginea.
At the 10 o'clock position of the dorsal mid-shaft of the penis, a hypoechoic oval structure consistent with a hematoma within the corpora cavernosa is noted adjacent to a 1.5 centimeter (cm) defect of the tunica albuginea (Figure 2, Figure 3, Figure 4, Video 1, Video 2).
Absence of signal when applying power Doppler over the lesion suggests no active bleeding (Video 3).
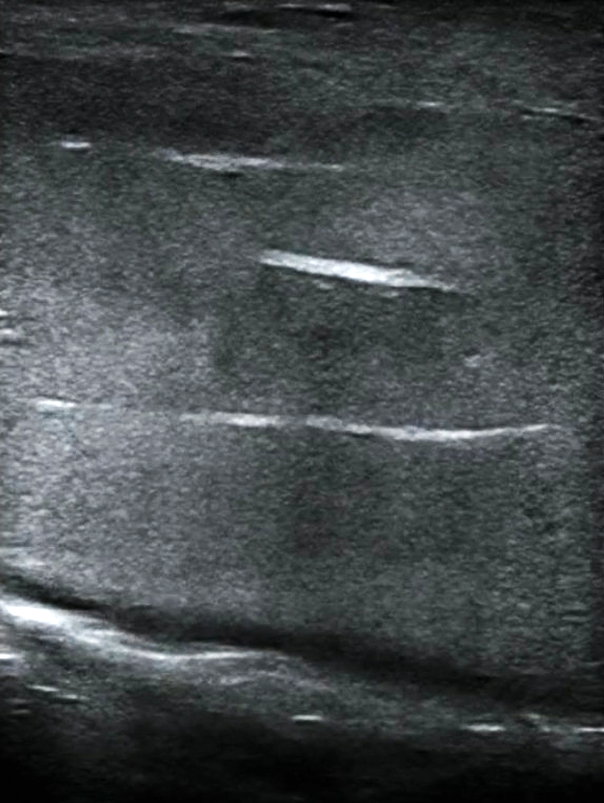
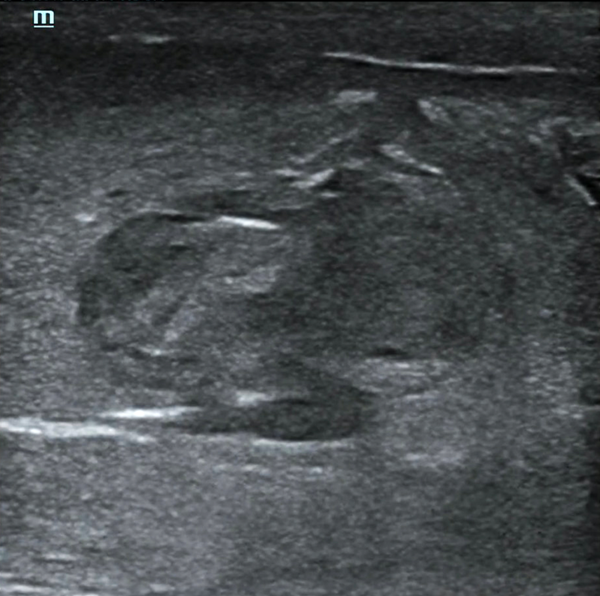
Figure 2. Point-of-care ultrasound of sagittal view showing normal anatomy of corpora cavernosa

Figure 3. Point-of-care ultrasound of sagittal plane of mid-shaft proximal penis demonstrating hematoma with edge artifact and TA defect
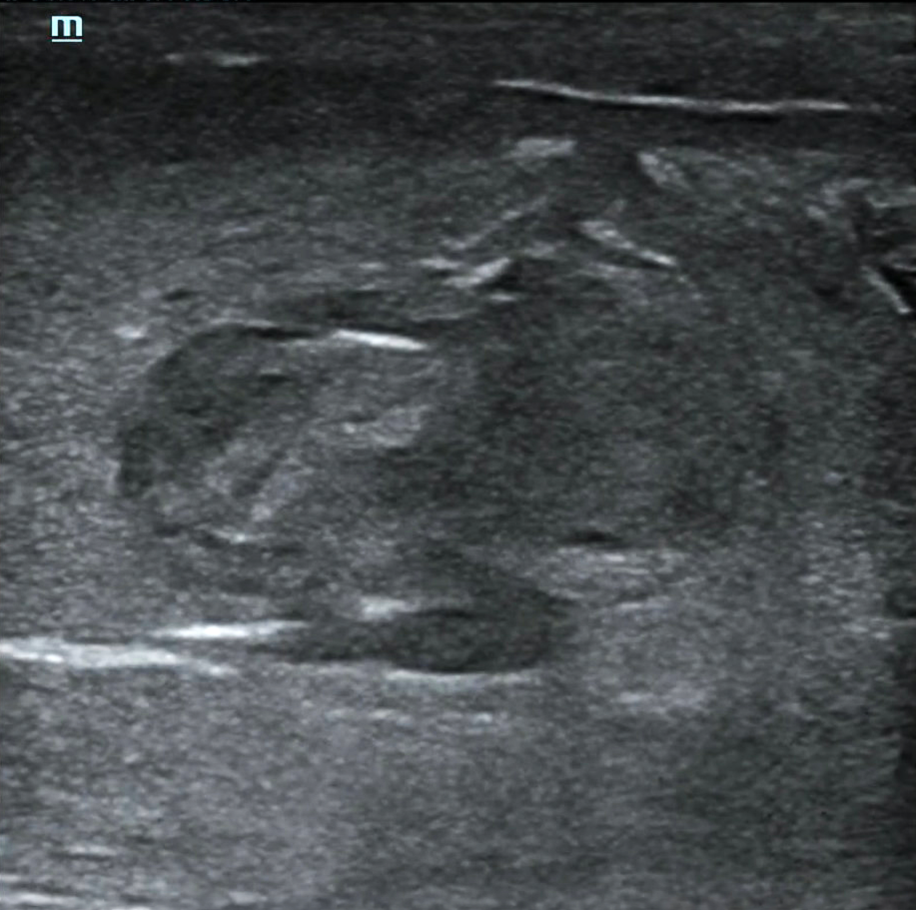
Figure 4. Point-of-care ultrasound of Transverse plane of mid-shaft proximal penis demonstrating hematoma and TA defect
Video 1. Point-of-care ultrasound of sagittal plane demonstrating hematoma with edge artifact and TA defect
Video 2. Point-of-care ultrasound of Transverse plane demonstrating hematoma and TA defect
Video 3. Point-of-care ultrasound of Transverse plane in Power Doppler demonstrating lack of flow
Discussion
A penile fracture is a rare urological emergency, with an estimated 500 – 600 cases reported annually in the United States. Approximately 50% of penile fractures occur during sexual intercourse while approximately 40% of the remaining cases are due to masturbation and forced flexion.1–3 It is caused by a rupture of the tunica albuginea fascia as the penis is forced into flexion during an erection. Classic presentations are described as an audible "snap" or "pop" followed by sudden detumescence, swelling, and penile pain.4 Upon examination, the penis can appear deviated and swollen due to the developing hematoma. Its appearance is referred to as an "aubergine sign" due to its similarities to an eggplant.5 Blood at the urethral meatus, as well as a urinalysis showing gross or microscopic hematuria, can indicate urethral injury and corpus spongiosum involvement.6–8
The penis is composed of two dorsally paired corpora cavernosa and the corpus spongiosum which lies ventral to the corpora cavernosa. Using ultrasound, the corpora cavernosa appears as a homogeneous, hypoechoic cylinders with a thin echogenic midline septum. The corpus spongiosum appears mildly more hypoechoic and is smaller in cross-section compared to corpora cavernosa. Surrounding the corpora cavernosa and the corpus spongiosum is the tunica albuginea which appears as a bright, hyperechoic line on transverse view or as a single-continuous band on sagittal view. Superficial to the tunica albuginea is Buck's fascia and Colles' fascia, appearing as thin hyperechoic lines (transverse). In a penile fracture, the tunica albuginea is ruptured and thus would be discontinuous at the point of the defect.9,10 Additionally, the hematoma in a penile fracture appears as a hypoechoic ovoid structure within the corpora cavernosa. If Buck's fascia is intact, the blood and hematoma remain confined to the cavernosal space. If Buck's fascia is also ruptured, blood proceeds to pool at the next fascia, Colles’ fascia, creating the ecchymosis that presents on the scrotum and perineum.11
Penile fractures can be diagnosed through ultrasound, magnetic resonance imaging (MRI), or surgical exploration. A retrospective cohort study evaluating the performance of ultrasound and MRI in patients with suspected penile fracture found ultrasound had a sensitivity and specificity of 94.6% and 93%, respectively.12 Additionally, ultrasound correctly confirmed the presence and marked the site of penile fracture in 92% of the patients that underwent surgical exploration and correctly identified urethral rupture in 92% of cases. In another retrospective review by Spiesecke et al., the sensitivity and specificity of MRI for detecting penile fractures were 91.9% and 90.6%, respectively, while ultrasound demonstrated a sensitivity of 71.4% and a specificity of 100%.13 While imaging should not delay surgical intervention, Stempl et. al's retrospective review of 193 patients presenting with clinical suspicion of penile fracture revealed 104 cases (54%) had an alternative diagnosis to penile fracture; 94 of the 104 cases had imaging suggest an alternative diagnosis and thus were not surgically explored. Notably, ultrasound suggested an alternative diagnosis in 76 out of the 94 cases (81%).
While penile fractures are traditionally considered a clinical diagnosis, the study by Stempl et. al highlights the challenges of accurate clinical diagnosis and the utility of POCUS in aiding diagnosis. Challenges with US imaging of the penis include technician ability, patient's inability to tolerate the scan, and gross swelling of the penis inhibiting adequate views of the tunica albuginea. However, POCUS's ubiquity and cost-effectiveness compared to MRI make it the recommended first-line tool for diagnosis in the emergency department.12,14
Hospital Course / Resolution
Urology was consulted, reviewed the POCUS scans with the ED team, and took the patient for urgent surgical intervention. After degloving of the penile skin and dissection down to the corpora cavernosum, a large hematoma was found to the proximal mid-shaft of the penis and was evacuated. A two cm defect in the tunica albuginea was found at the 10 o’clock position of the dorsum mid-phallus and closed with 3-0 vicryl. The patient was sent to the Post-Anesthesia Care Unit (PACU) for recovery and discharged that same morning.
The patient made a full recovery with no genitourinary complications and resumed sexual activity 3 weeks later.
References
- Aaronson DS, Shindel AW. U.S. National Statistics on Penile Fracture. The Journal of Sexual Medicine. 2010;7(9):3226.
- Masarani M, Dinneen M. Penile fracture: diagnosis and management. Trends in Urology, Gynaecology & Sexual Health. 2007;12(5):20-24.
- Rodriguez D, Li K, Apoj M, Munarriz R. Epidemiology of Penile Fractures in United States Emergency Departments: Access to Care Disparities May Lead to Suboptimal Outcomes. The Journal of Sexual Medicine. 2019;16(2):248-256.
- Koifman L, Barros R, Júnior RAS, Cavalcanti AG, Favorito LA. Penile Fracture: Diagnosis, Treatment and Outcomes of 150 Patients. Urology. 2010;76(6):1488-1492.
- Al‐Shaiji TF, Amann J, Brock GB. Fractured Penis: Diagnosis and Management (CME). The Journal of Sexual Medicine. 2009;6(12):3231-3240.
- Amit A, Arun K, Bharat B, Navin R, Sameer T, Shankar DU. Penile fracture and associated urethral injury: Experience at a tertiary care hospital. Can Urol Assoc J. 2013;7(3-4):E168-E170.
- Penson DF, Seftel AD, Krane RJ, Frohrib D, Goldstein I. The hemodynamic pathophysiology of impotence following blunt trauma to the erect penis. J Urol. 1992;148(4):1171-1180.
- El Atat R, Sfaxi M, Benslama MR, et al. Fracture of the Penis: Management and Long-Term Results of Surgical Treatment. Experience in 300 Cases. Journal of Trauma and Acute Care Surgery. 2008;64(1):121.
- Nomura JT, Sierzenski PR. Ultrasound Diagnosis of Penile Fracture. The Journal of Emergency Medicine. 2010;38(3):362-365.
- Fernandes MAV, de Souza LRMF, Cartafina LP. Ultrasound evaluation of the penis. Radiol Bras. 2018;51(4):257-261.
- Kamdar C, Mooppan UMM, Kim H, Gulmi FA. Penile fracture: preoperative evaluation and surgical technique for optimal patient outcome. BJU International. 2008;102(11):1640-1644.
- von Stempel C, Kirkham A, Cayetano Alcaraz A, et al. Imaging findings in suspected penile fracture: alternative diagnoses and surgical correlation. British Journal of Radiology. 2024;97(1163):1850-1855.
- Spiesecke P, Mang J, Fischer T, Hamm B, Lerchbaumer MH. Diagnostic performance of MRI and US in suspicion of penile fracture. Transl Androl Urol. 2022;11(3):377-385.
- Shukla AK, Bhagavan BC, Sanjay SC, Krishnappa N, Sahadev R, V. S. Role of Ultraosonography in Grading of Penile Fractures. J Clin Diagn Res. 2015;9(4):TC01-TC03.