Unintentional injury continues to be one of the major causes of morbidity and mortality in the pediatric age group, with urogenital injury occurring in 10-20% of blunt abdominal trauma cases.1,2
Depending on the severity, the short-term complications of renal trauma can include hemorrhage, sepsis, perinephric abscess, fistula, and urinary extravasation, and long-term consequences can include renal failure and unrelenting hypertension.3
Management of these patients can be intimidating and require significant interdisciplinary coordination among urologists, interventional radiologists, trauma surgeons, and intensivists. With emergency physicians often serving as the mediator in these situations, it is imperative to familiarize oneself with evidence-based guidelines, and we hope to help provide some tools in this article.
Case
A 13-year-old male presented to our emergency department via EMS secondary to blunt trauma to the right flank in a football game resulting in severe right-sided abdominal and flank pain. While jumping, he was struck in his right side by another player’s knee and then fell to the ground. He was unable to stand or ambulate on his own, but he did not lose consciousness or hit his head. There was no other trauma sustained at that time. On arrival, he was awake, alert, and oriented with 10/10 right abdominal and flank pain localized over the 11th and 12th ribs. He denied any other pain. Physical exam demonstrated hemodynamic stability and severe tenderness to palpation of the right abdomen and right flank with no overlying ecchymosis. There was no diffuse abdominal tenderness, distension, or guarding that would suggest an acute abdomen.
Given the site of injury, we had a high index of suspicion for injury to the ribs, liver, and kidney. Chest X-ray did not demonstrate rib fractures or pneumothorax. Focused Assessment with Sonography for Trauma (FAST) exam demonstrated loss of normal right kidney architecture with equivocal perinephric fluid collections with no signs of intraperitoneal fluid collection (Figure 1). A retroperitoneal ultrasound of the right kidney was ordered and showed an enlarged kidney with evidence of complex renal laceration and perinephric hematoma as well as minimal blood flow within the renal hilum on color Doppler. Three hours after initial presentation, a CT abdomen/pelvis with IV contrast demonstrated a grade IV/V right kidney laceration extending into the renal hilum with a large perinephric hematoma (Figure 2). No excreted contrast was seen outside of the renal collecting system on delayed imaging, and there was low suspicion at that time for ureteral injury.
Figure 1. RUQ ultrasound demonstrating loss of normal renal architecture

Figure 2. Abdominal CT imaging showing a large right perinephric hematoma
Because of the grade IV/V renal injury, the patient was admitted to the surgical trauma intensive care (SICU) unit for close monitoring, including frequent hemoglobin checks and serial abdominal examinations. Interventional radiology recommended conservative management without embolization or drainage of the perinephric hematoma. His SICU stay was uneventful with stable hemoglobin and hemodynamics. He was discharged to the floor on day three where a repeat CTA abdomen/pelvis showed partial devascularization of the right inferior pole of the kidney as well as contrast extravasation consistent with a renal pelvis injury. Interventional radiology was again consulted for possible percutaneous nephrostomy tube placement but declined due to the risks associated with procedures on abnormal renal architecture and possible loss of tamponade effect. Urology was consulted and a right ureteral stent was placed to assist with drainage of the collecting. A third CTA abdomen/pelvis on hospitalization day eight demonstrated decreased urine extravasation, and the patient was discharged on day nine with close urology follow-up.
Discussion
There is a 10-20% incidence of urogenital trauma, with the kidney being the most commonly affected organ. Ninety percent of blunt kidney injuries are associated with high-velocity deceleration with mechanisms like major falls, motor vehicle accidents, or sports injuries.3 Additionally, children and adolescents are more likely to suffer renal injury than adults following motor vehicle accidents.4 The kidney’s fixation only to the renal pelvis and the highly vascular pedicle makes it prone to insult, but the vast majority are minor.
As emergency physicians in both adult and pediatric settings, it is important to use an informed and standardized approach in the evaluation and treatment of a patient like the one in this case. The American Urological Association (AUA)’s guidelines for urotrauma management steered the establishment of a multidisciplinary set of recommendations from the World Society of Emergency Surgery (WSES) and the American Association for the Surgery of Trauma (AAST), involving urologists, interventional radiologists, trauma surgeons, emergency physicians, and intensivists. Expectedly, urologists and trauma surgeons can have differing priorities when choosing their ideal management in an ill patient, so this collaborative, evidence-based, published advice can help guide the team toward the best outcome for the patient and their urological organs.
Presentation
Clinical examination should consider the presence of hematuria, flank/abdominal pain/contusion, rib fractures, pelvic injury, and mechanism of trauma. It is important to remember that children are more vulnerable to blunt kidney injury due to less perirenal fat, thinner abdominal muscles, lack of ossification of the rib cage, larger kidney size, and fetal kidney lobulations. Non-operative management (NOM), especially in pediatric patients, is preferred unless the patient is hemodynamically unstable or has an expanding retroperitoneal hematoma, which would prompt emergent surgery or interventional radiology consultation.3,5,6
Evaluation
If the patient is hemodynamically stable, further workup must take place, including CBC, CMP, and UA. While FAST exams are effective at rapid identification of intra-abdominal free fluid, they have low sensitivity (22-67%, depending on level of expertise) in kidney trauma. Therefore, contrast-enhanced CT scan associated with delayed urographic phase is the gold standard for adults and children with deceleration mechanism of injury or hematuria with hypotension. Delayed urographic phase imaging is particularly useful in evaluating injury to the urinary collecting system.5 For stable pediatric or pregnant patients with hematuria of <50 RBCs, ultrasound and close clinical monitoring can be used, but be aware of its limitations. CT scans showing at least two of the following criteria with high-grade injury (AAST III-V, Figure 3) have a high likelihood of failing NOM and requiring earlier and more aggressive intervention: contrast blush, perirenal hematoma >3.5cm, medial laceration with extravasation, and lack of contrast in the ureter. 5,6
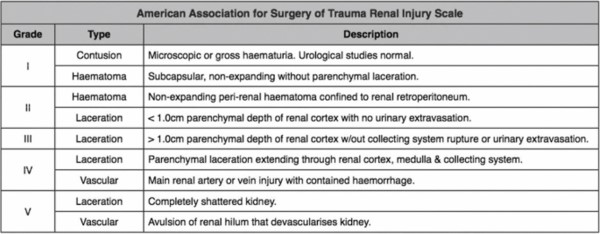
Figure 3. AAST grading criteria for renal injury
Management
NOM is the treatment of choice for all hemodynamically stable patients as it leads to higher renal preservation rate, shorter hospital stays, and comparable complication rate to operative management (OM). CT image-guided classification of injury severity can help determine a stepwise approach from conservative management to minimally invasive intervention to laparotomy. It is reasonable to consider NOM in severe injuries at tertiary centers where close monitoring and immediate interventional resources are available, and it may be continued following angioembolization of injury.
In the unstable patient, treatment should include OM, and Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) can bridge to definitive procedures if necessary.
In pediatric patients, angioembolization is the first choice for intervention if resources allow, as the reported success rate and morbidity rate is 100% and 0% respectively for pseudoaneurysm or contrast medium extravasation.5 A comprehensive algorithm from WSES/AAST can be seen in Figure 4.
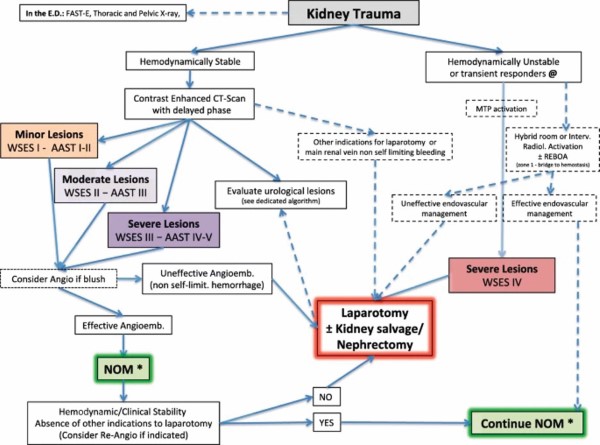
Figure 4. WSES/AAST algorithm for the diagnosis and management of renal trauma
Outcomes
Complications to blunt renal injury can be seen in the hospital setting or in follow-up visits to the emergency department. For example, renal ischemia can lead to unrelenting hypertension due to activation of renin-angiotensin-aldosterone system. In addition, secondary hemorrhage is fairly common (25% of moderate/severe injuries) and can occur within two weeks of the initial insult. A nephrectomy is required in about 4% of blunt renal injury patients and is associated with a 4.58-fold increased risk of acute kidney injury with decreased renal function.7,8 In contrast, transarterial embolization is not a risk factor for AKI.7 A patient can return to sports activities when microscopic hematuria is resolved, likely 2-6 weeks for mild to moderate injuries and 6-12 months for more severe injuries.
Our Patient
This adolescent patient demonstrates a classic presentation of a high-grade blunt renal injury with severe flank pain and a clear mechanism of injury. It was prudent to obtain FAST imaging to assess for intraperitoneal bleeding as well as chest X-rays to assess for pneumothorax and rib fractures; however, as discussed, these modalities have low sensitivity for renal injury.
Contrasted CT imaging with delayed phase imaging would have been the best diagnostic next step, but these images were not obtained until three hours after arrival. Urology was not officially consulted until day five of admission after repeat imaging demonstrated injury to the renal pelvis. Despite the severity of the renal injury, non-operative management with close observation was the appropriate initial choice for our patient due to his hemodynamic stability. Surgical management remained conservative with no surgical interventions pursued aside from ureteral stent placement to help divert the extravasation of urine.
Our patient continued to follow-up with urology frequently after discharge. His only reported symptoms in the months after his hospitalization were infrequent crampy pain in his right flank. A repeat CT of the abdomen and pelvis with contrast one month post-discharge showed decreasing size of the right perinephric fluid collection with a devascularized right lower pole; CT imaging two months post-discharge showed complete resolution of the perinephric fluid collection. A ureteral stent was left in place until three months after initial placement, at which time it was removed uneventfully. To date, there have been no signs of persistent hypertension, and renal function has returned to baseline. Our patient has been cautioned about the risk of returning to football and the need to wear an abdominal guard if he does choose to continue playing.
In summary, the choices made in this case were in accordance with WSES/AAST guidelines and resulted in a positive patient outcome. In the future, we can improve by obtaining CT imaging with delayed phase more rapidly in hemodynamically stable patients and by facilitating an early interdisciplinary approach to patient care, including urology, trauma surgery, and interventional radiology.
References
- Cunningham RM, Walton MA, Carter PM. The major causes of death in children and adolescents in the United States. N Engl J Med. 2018;379(25):2468-2475.
- Petrone P, Perez-Calvo J, Brathwaite CEM, Islam S, Joseph DK. Traumatic kidney injuries: A systematic review and meta-analysis. Int J Surg. 2020;74:13-21.
- Singer G, Arneitz C, Tschauner S, Castellani C, Till H. Trauma in pediatric urology. Semin Pediatr Surg. 2021;30(4):151085.
- Kurtz MP, Eswara JR, Vetter JM, Nelson CP, Brandes SB. Blunt Abdominal Trauma from Motor Vehicle Collisions from 2007 to 2011: Renal Injury Probability and Severity in Children versus Adults. J Urol. 2017;197(3 Pt 2):906-910.
- Coccolini F, Moore EE, Kluger Y, et al. Kidney and uro-trauma: WSES-AAST guidelines. World J Emerg Surg. 2019;14:54. Published 2019 Dec 2.
- Morey AF, Broghammer JA, Hollowell CMP, McKibben MJ, Souter L. Urotrauma Guideline 2020: AUA Guideline. J Urol. 2021;205(1):30-35.
- Noorbakhsh A, Aganovic L, Vahdat N, Fazeli S, Chung R, Cassidy F. What a difference a delay makes! CT urogram: a pictorial essay. Abdom Radiol (NY). 2019;44(12):3919-3934.
- Hsu CP, Cheng CT, Huang JF, et al. The effect of transarterial embolization versus nephrectomy on acute kidney injury in blunt renal trauma patients. World J Urol. 2022;40(7):1859-1865.
- Wright JL, Nathens AB, Rivara FP, Wessells H. Renal and extrarenal predictors of nephrectomy from the national trauma data bank. J Urol. 2006;175(3 Pt 1):970-975.



