POCUS is a key diagnostic tool that can allow emergency physicians to diagnose a range of injuries. This case explains how to identify a molar pregnancy in the emergency department.
Faculty editor: Ochan Kwon, MD
HISTORY OF PRESENT ILLNESS
A 21-year-old female, G3P1011, presented to the emergency department with complaints of vaginal bleeding and lower abdominal cramping that started 1 month ago and have been worsening over the last 3 days. Patient notes using 7 pads a day during the last 3 days, and describes passing bright red clots. She believes she is pregnant based on her abdomen getting bigger and the sensation of fetal movement, although she has not taken a pregnancy test. Her last menstrual period was in 2 months ago in June. She denies nausea, vomiting, diarrhea, urinary symptoms, back pain, or any other symptoms.
PHYSICAL EXAMINATION
Vital signs: T 97.6°F, HR 76 bpm, BP 130/88 mmHg, RR 19/min, SpO₂ 99% on room air.
On exam, the patient is visibly distressed due to the vaginal bleeding. Her abdominal exam reveals a gravid abdomen with mild suprapubic tenderness. Her skin is warm and she is alert and oriented x3. ED bedside pelvic exam reveals copious bright red blood clots filling the vaginal vault, once the clots were evacuated, the cervix appears open and expelling clots.
Labs and Imaging
Labs reveal hemoglobin of 8.5 g/dL and a β-hCG level of 742,714. Rest of labwork within normal limits.
POCUS
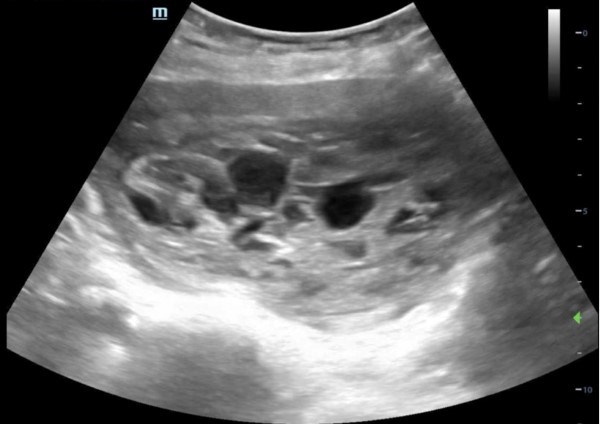
Bedside transabdominal POCUS was performed using a curvilinear probe with the OB preset selected. A heterogeneous intrauterine mass with numerous small anechoic cystic structures was visualized. This classic appearance of a molar pregnancy is often described as a "snowstorm" or "cluster of grapes" pattern due to the presence of several hypoechoic structures that represent the multiple hydropic villi. There is no fetal tissue visible. Additionally, at the fundus of the uterus (left side of the picture), there is a separation of the mass from the uterine lining signified by an anechoic line.
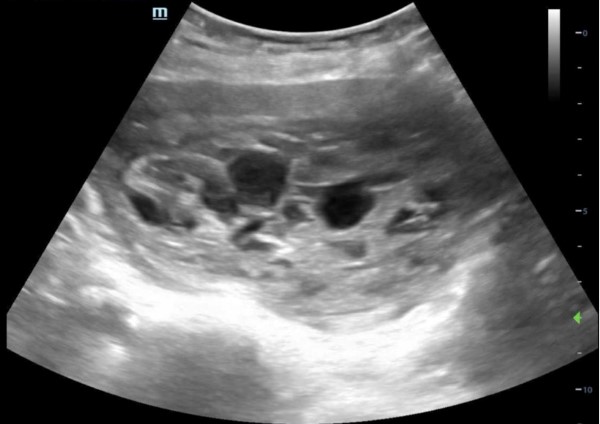
Figure 1. Transabdominal ultrasound in the transverse plane demonstrating snowstorm appearance consistent with molar pregnancy.
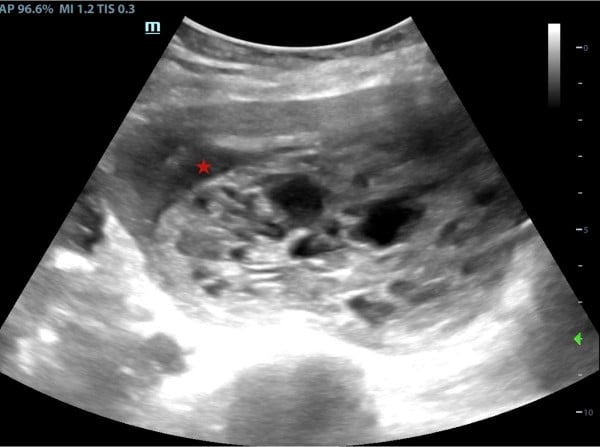
Figure 2. Transabdominal ultrasound in the transverse plane showing the separation of the mass and the uterine lining shown by the anechoic line (see star)
Video 1. Ultrasound findings upon exam
Discussion
Molar pregnancy is a rare form of gestational trophoblastic disease occurring in about 1 in 1000 pregnancies.1 It results from abnormal fertilization and is classified as complete or partial mole, with complete moles lacking fetal tissue and partial moles containing abnormal embryonic tissue.2 Patients typically present in the first trimester with vaginal bleeding, an enlarged uterus, and elevated β-hCG levels.3 While physical exam and serum markers are important, they lack specificity in diagnosis.
Point-of-care ultrasound is increasingly valuable in the emergency department for early identification of molar pregnancy. The classic ultrasound finding in complete moles is a heterogeneous intrauterine mass with multiple cystic spaces, often described as a "snowstorm" or "cluster of grapes" appearance, and typically lacking fetal or embryonic tissue.4 In contrast, partial moles often display fetal parts, a gestational sac, and an enlarged placenta with focal cystic changes often referred to as a "Swiss cheese" pattern.2 Sensitivity of POCUS for detecting complete moles is high (90%), though partial moles and early disease may be more difficult to identify due to less distinct sonographic features.5 Other imaging modalities like CT or MRI are rarely used initially but may assist in complex cases or metastatic evaluation.
Despite its advantages, POCUS has limitations. Operator skill significantly influences diagnostic accuracy, and findings can overlap with retained products of conception or incomplete abortion. Early or partial moles often lack the classic ultrasound appearance, reducing sensitivity.6
Management involves urgent gynecologic consultation and uterine evacuation, usually by dilation and curettage (D&C). After evacuation, serial β-hCG monitoring is critical to detect persistent disease or malignancy. Contraceptive use during this period is advised to ensure accurate interpretation of hCG trends.7
Hospital Course/Resolution
The patient remained hemodynamically stable despite heavy vaginal bleeding. OB/GYN was consulted and patient was taken to the OR for surgical evacuation of a complete mole. Patient required 3 units of blood prior to OR due to worsening tachycardia and symptomatic treatment in the setting of large volume blood loss. D&C was successful, and the patient was discharged home after 2 days.
References
- Gestational trophoblastic disease. Chapter 3: Epidemiology. International Society for the Study of Trophoblastic Diseases. 5th ed, 2022.
- Berkowitz RS, Goldstein DP. Clinical practice. Molar pregnancy. N Engl J Med. 2009 Apr 16;360(16):1639-45.
- Ngan HYS, Seckl MJ, Berkowitz RS, et al. Diagnosis and management of gestational trophoblastic disease: 2021 update. Int J Gynaecol Obstet. 2021 Oct;155 Suppl 1:86-93.
- Fowler DJ, Lindsay I, Seckl MJ, Sebire NJ. Routine pre-evacuation ultrasound diagnosis of hydatidiform mole: experience of more than 1000 cases from a regional referral center. Ultrasound Obstet Gynecol. 2006 Jan;27(1):56-60.
- Johns J, Greenwold N, Buckley S, Jauniaux E. Ultrasound screening for molar pregnancies in missed miscarriages. Ultrasound Obstet Gynecol. 2005 May;25(5):493-8.
- Ngan HYS, Seckl MJ, Berkowitz RS, et al. Diagnosis and management of gestational trophoblastic disease: 2021 update. Int J Gynaecol Obstet. 2021 Oct;155 Suppl 1:86-93.
- Berkowitz RS, Goldstein DP. Current advances in the management of gestational trophoblastic disease. Gynecol Oncol. 2013 Apr;128(1):3-7.