Special Events Special
• Part 1
Introduction to Mass Gatherings
As highly social creatures, mass gathering are an integral part of our lives. From sporting events to concerts, these events present a unique set of circumstances regarding public health and safety. A mass gathering can be defined as an event during which crowds gather and where there is a potential for a delayed response to emergencies because of limited access to patients or other features of the environment and location.1 These events often strain local emergency medical services (EMS) systems as well as nearby hospitals, especially when there is poor planning and lack of medical resources. Without clear guidelines in place, many jurisdictions face a considerable challenge when presented with planning the medical care for these events. In addition, most of the ideas and recommendations presented in the literature are based on “expert opinion” as opposed to scientific evidence.2 Emergency physicians, and emergency medical services (EMS) physicians in particular, are well-positioned to estimate the medical resources needed to support these large events.
Challenges to Mass Gathering Medical Care
Mass gatherings pose a variety of challenges, from preplanning through execution as well as postevent analysis. The current literature concerning mass gatherings has abundant retrospective information on the medical presence and outcomes at a variety of events, but lacks a general consensus on the specific resources necessary for a prospective event. A number of models have been created in an effort to estimate the emergency medical resources required for an event based on multiple variables. Hartman, et al, identified five factors that affect patient presentation, specifically weather, attendance, ethanol presence, crowd age, and crowd intention, in an attempt to stratify events into minor, intermediate or major categories.3 The Arbon model predicts patient presentations based on specific variables present at a wide range of events.4 The model indicated that the patient presentation rate (PPR), often presented as the number of presenting patients per 1,000 event attendees, had a positive relationship with crowd size, relative humidity, sale of alcoholic beverages, and number of medical personnel at the event. Attempts to validate these models have shown they have some utility in predicting patient presentations, but fall short when predicting patient transfers to local hospitals and the requisite number and type of medical resources.2,5,6
Particular events pose unique obstacles, and these must be identified in the planning stages in order to allocate resources properly. Marathons, for example, present an unbounded and unfocused crowd with a larger number of participants than spectators, requiring careful planning of resources at optimal points along the race and mobility of care teams to augment the further distance stations.7 Sporting events may present a low PPR but a higher rate of cardiac arrests, while a rock concert may have a high PPR with very few cardiac arrests.8 The most common reasons for seeking medical care include dermal and musculoskeletal injuries, heat-related illness and dehydration, gastrointestinal complaints, and headaches.911 A common patient complaint at concerts is drug overdose, and knowing the pattern of drug use in the region as well as at a particular event will allow providers to anticipate critical presentations. Predicting the prevalent complaints based on event variables may help guide planning the level of care, personnel, facility placement and equipment necessary.
Probably the most frustrating aspect of planning mass gathering medical care is the lack of standardization and guidelines in most jurisdictions. Only a handful of states have existing regulations, with no uniformity of planning or medical care. It is a common misconception that mass gathering medical care is analogous to routine EMS practice, while in reality mass gatherings present unique challenges that require special planning and often a broadened scope of practice. Sanders, et al, provided recommendations including basic first aid and life support within 4 minutes of a patient becoming ill, and advanced life support resuscitation within 8 minutes of a patient becoming ill.12 The authors suggest that nonphysician medical care providers should not treat nonemergent problems or render judgment without direct supervision of a licensed physician. Standardized legislation regarding mass gathering medical care is a necessity if participants and spectators are expected to receive uniform access to competent emergency medical care, and physicians are in a position to both write and promote such legislation.
The Role of the Physician in Mass Gatherings
The concept of physician presence and supervision during a mass gathering is not unique. As early as 1979, physicians have been identified as a crucial element to effective and medically sound emergency medical service.13 MartinGill, et al, reported that while physician presence led to an absolute increase in patient census and transports, a decrease in the percent of patients transported was seen with likely minimal impact on local EMS and emergency department resources.14 A sporting event experienced a low rate of ambulance transfers to local hospitals, and the authors concluded this finding was likely related to the ability of medical doctors to treat and discharge patients if deemed stable.15 Direct physician oversight may increase treatandrelease rates, as prehospital providers cannot typically perform this function.16 The physician's ability to finalize disposition of patients onsite is critical to off-loading local EMS system and emergency department resources outside the event.17 In addition, physician presence is invaluable at events where the transport distance and times to definitive care is considerable, allowing patients to receive a higher level of care at the time of presentation.18 Beyond the obvious ability to treat patients during the event, physician oversight can be useful throughout the planning stages. The National Association of EMS Physicians' position paper on mass gathering care reviews the particulars of medical action plan.19 An effective medical plan should outline the responsibilities of physicians assigned to the event, detail the scope of event medical care, and comprehensively address issues related to onsite communications, medical equipment, physician oversight, and resource allocation. It is important for a physician to be involved from the beginning of the process to facilitate protocols for nonphysician personnel and help create a plan that provides patients with the highest quality care possible. Without direct physician oversight, elective nontransport of patients by EMS crews is considered risky.17 Sanders, et al, proposed guidelines recommending 12 physicians for every 50,000 people,12 and consideration of the event type may necessitate additional physician presence.
Paramedics remain an invaluable resource at mass gatherings, and providing them with written directives unique to a particular mass gathering can allow them to manage patients who would otherwise require transfer to a hospital. Paramedicstaffed rehydration units have been used,20 and at times when physician resources are limited, physicians can provide structured treat-andrelease protocols utilizing overthecounter medications.21 Everyday EMS systems are inadequately equipped to evaluate and release patients, and by following usual directives many patients would require transfer, further straining the EMS system and local hospitals. By providing these protocols to address a variety of patient presentations common to a distinct type of mass gathering, paramedics may be maximally utilized and in doing so allow onsite physicians to be available for treatment of more critically ill patients.
The specialty of the physician involved in a special event should also be considered, and emergency physicians are uniquely qualified for this role. By virtue of their expertise and training, emergency physicians can comfortably provide an increased level of care at such events. A seemingly untapped resource is the presence of emergency medicine residents at mass gatherings.22 Not only will their participation promote comprehensive care at events, but also it may foster an enduring commitment to participating in prehospital care and provide community leaders to further develop the emergency medical system. By becoming involved in mass gathering medical care, emergency physicians in any stage of their career can contribute to their local EMS system and help elevate the care provided at these events.
Practical Considerations: The Baltimore Grand Prix
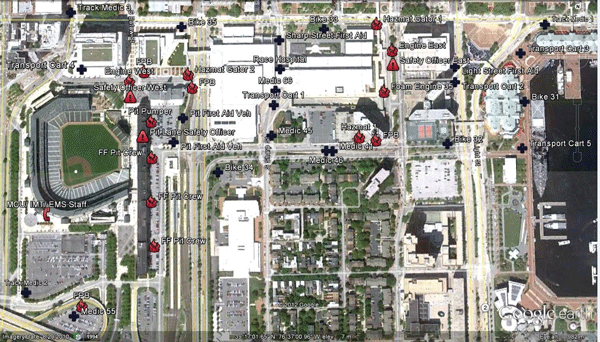
The Baltimore Grand Prix was one event that thrust physician involvement in mass gathering care into the spotlight.6 From 2011-2013, this mass gathering event drew crowds in excess of 100,000 to the metropolitan Baltimore area and threatened to further strain the already overtaxed emergency medical services system. The sheer scope of the event necessitated a novel approach to emergency care; simply scheduling another six ambulances to operate during the event would not meet the projected demand. Event planners and medical directors worked to create a “closed EMS system” tailored to the unique geographic and operational constraints of the Grand Prix. Thousands of spectators were located within a fencedin barrier, and ambulances had to be prepositioned at strategic locations. Resources were allocated to ontrack emergency care, and spectator services consisted of a deployment of physicianstaffed first aid stations. Finally, a standalone “race hospital” was deployed to focus on the urgent and emergent needs of Grand Prix racers and staff. The hospital was staffed with Grand Prix physicians, an Xray machine, resuscitation equipment, and common urgent care medicines. A mobile command unit provided dispatch and communication services for responding units assigned to the event. The preplanning was instrumental in minimizing the event's impact upon an already under-resourced EMS jurisdiction. This event clearly illustrated the diverse challenges posed by estimating resources for mass gatherings, and the success of the event was in large part due to the careful planning and coordinated interaction between EMS providers and participating physicians.
Conclusion
Physician involvement is key to the effective planning and provision of mass gathering medical care, and participating physicians should be appropriately trained in emergency care and be comfortable while interacting with prehospital providers. Emergency medicine physicians, including residents, are well positioned to not only provide definitive medical care at events, but also to get involved in regional legislation regarding mass gathering medical care. The EMS subspecialty of emergency medicine allows physicians to obtain specific training in prehospital emergency patient care, making them highly qualified to aid and advise appropriate medical care for mass gatherings, as well as provide medical oversight of EMS activities during these events. Without consistent guidelines and close medical oversight, EMS systems are left to provide usual care instead of preparing a medical plan tailored to the needs of the event. Becoming involved in event medicine can be a rewarding way to provide high quality care as well as help shape future mass gathering medical care.
References
- Arbon P. Mass gathering medicine: a review of the evidence and future directions for research. Prehosp Disaster Med 22(2):131135, 2007.
- Zeitz KM, Zeitz CJ, Arbon P. Forecasting medical work at massgathering events: Predictive model versus retrospective review. Prehosp Disaster Med 20(3): 164168, 2005.
- Hartman N, Williamson A, Sojka B, et al. Predicting resource use at mass gatherings using a simplified stratification scoring model. Am J Emerg Med 27(3):337343, 2009.
- Arbon P, Bridgewater FH, Smith C. Mass gathierng medicine: a predictive model for patient presentation and transport rates. Prehosp Disaster Med 16(3):150158, 2001.
- Smith WP, Tuffin H, Stratton SJ, et al. Validation of a modified medical resource model for mass gatherings. Prehosp Disaster Med 28(1):1622, 2012.
- Nable JV, Margolis A, Lawner B, et al. Comparison of prediction models for use of medical resources at urban autoracing events. Prehosp Disaster Med 29(6):608613, 2014.
- Nguyen R, Milsten A, Cushman J. Injury patterns and levels of care at a marathon. Prehosp Disaster Med 23(6):516525, 2008.
- Michael J, Barbera J. Mass gathering medical care: a twentyfive year review. Prehosp Disaster Med 12(4):305312, 2008.
- Milsten A, Seaman K, Liu P, et al. Variables influencing medical usage rates, injury patterns, and levels of care for mass gatherings. Prehosp Disaster Med 18(4):334346, 2003.
- Soomaroo L, Murray, V. Weather and environmental hazards at mass gatherings. PLoS Curr Jul 31;4, 2012.
- Grant WD, Nacca NE, Prince L, et al. Massgathering medical care: retrospective analysis of patient presentations over five years at a multiday mass gathering. Prehosp Disaster Med 25(2):183187, 2010.
- Sanders A, Criss E, Steckl P, et al. An analysis of medical care at mass gatherings. Ann Emerg Med 15(5):515519, 1986.
- Gunter M, Ricci E, Silverman M, et al. Physician involvement: a critical factor in the development of community emergency medical services. Emerg Med Serv 8(3):48, 5055, 5760, 1979.
- MartinGill C, Brady WJ, Barlotta K, et al. Hospitalbased healthcare provider (nurse and physician) integration into an emergency medical servicesmanaged massgathering event. Am J Emerg Med 25(1):1522, 2007.
- Hardcastle TC, Samlal S, Naidoo R, et al. A redundant resource: a preplanned casualty clearing station for a FIFA 2010 stadium in Durban. Prehosp Disaster Med 27(5):409415, 2012.
- Grange J, Baumann G, Vaezazizi R. Onsite physicians reduce ambulance transports at mass gatherings. Prehosp Disaster Med 7(3):322326, 2003.
- De Lorenzo R. Mass gathering medicine: a review. Prehosp Disaster Med 12(1):6872, 1997.
- Parrillo S. Medical care at mass gatherings: considerations for physician involvement. Prehosp Disaster Med 10(4):273275, 1995.
- Jaslow D, Yancy A, Milsten A. Mass gathering medical care. Prehosp Disaster Med 4(4):359360, 2000.
- Lukins J, Feldman M, Summer J, et al. A paramedicstaffed medical rehydration unit at a mass gathering. Prehosp Disaster Med 8(4):411416, 2004.
- Feldman MJ, Lukins, JL, Verbeek PR, et al. Use of treatandrelease medical directive for paramedics at a mass gathering. Prehosp Emerg Care 9(2):213217, 2005.
- Ray AM, Sole DP. Emergency medicine resident involvement in EMS. J Emerg Med 33(4):385394, 2007.