Since the 1920s, 54 countries have had great success utilizing specialty-trained dental therapists to provide dental care in their communities.
Non-traumatic dental pain (NTDP) is a frequent chief complaint encountered by the emergency medicine resident. Recent publications demonstrate an increasing number of patients relying on the ED for their dental care.1-4 Between 2006 and 2009, there was a 15.8% increase in visits to the ED for NTDP.2
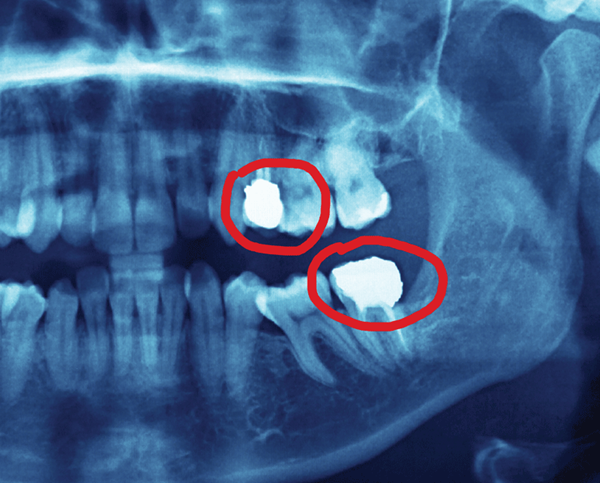
The treatment of patients with NTDP is often a nerve block and/or an opiate prescription. However, untreated (or under-treated) dental conditions can progress to serious infections, such as Ludwig's angina and cavernous sinus thrombosis.5-7 Despite the possibility of progression to these dangerous conditions, the EM literature is focused on curtailing opiate prescriptions, rather than focusing on interventions to treat the associated disease.8 In one retrospective study of NTDP visits, 90% of patients had no procedure performed, and 81% were prescribed opiates.4 As the number of opiate prescriptions rises and the rate of recidivism increases, it is not difficult to recognize a growing problem.9
Access to dental care varies depending on where a practice is located. Dental-related ED visits occur twice as frequently in rural areas as they do in large metropolitan areas. This is one reason why EM residents training at large academic centers may be blinded to this growing dilemma.2 Furthermore, the rate of NTDP ED visits is more than four times greater among patients from the lowest income communities than for patients in the highest income communities.2
The specialty of EM has roots grounded in public health. Through the twentieth century, medical specialties were created as the fund of knowledge increased; scientific discoveries beget doctors to deliver specialized care to the public. In contrast, emergency medicine was born out of public need. To this day, patients come to our doors when they need care the most. The role of emergency physicians likely will continue to change as we aim at the ever-moving target of public health needs.
This changing health care climate has stressed the importance of EM residents becoming stewards of patient health while maintaining concern for costs associated with the care we deliver. Costs rise dramatically when dental care is provided in the hospital setting.11 In fact, research shows a ten-fold increase in costs over dental office-based preventative care for Medicaid enrollees who required inpatient treatment for oral conditions.12 Focusing on creating cost-conscious solutions to close the growing gap in dental coverage should become a goal of emergency physicians, dentists, and policymakers alike.
Proposed solutions
In 2004, the American Dental Association estimated there were 183,430 dentists practicing in our country. Unfortunately, less than 1% of them practice in rural areas.13 Educating a greater number of dentists would seem to be the easiest fix, but this does not happen overnight;14 and less than 0.5% of new dental school graduates choose to practice in rural areas.13 The situation seems to mirror the lack of primary care physicians being produced by medical schools throughout the country.15
As a solution, both Minnesota and Alaska have created intensive educational programs aimed at advancing experienced dental hygienists into mid-level dental provider positions.16,17 It is unknown how this initiative has directly impacted the frequency of NTDP in hospital emergency rooms, yet it can be inferred that — with better preventative care — many visits to the ED can be avoided. Since the 1920s, 54 countries have had great success utilizing similar specialty-trained dental therapists to provide dental care in their communities.18
Unfortunately, despite success utilizing mid-level providers, many states have opposed these measures. Due to a combination of money, politics, and lack of awareness, these legislations fall off the docket with little public knowledge of their coming and going. Rather than work together, professional organizations spend considerable time and energy fighting in the political coliseum instead of building a solution to this growing problem.
Should EM residents promote the use of mid-level providers in dentistry? If our specialty prides itself in advocating strongly for patients within the walls of our EDs, why should we not support them in our state legislatures? The 2011 ACGME program requirements for graduate medical education in EM states, “Residents are expected to advocate for quality patient care and optimal patient care systems.”19 By showing support, EM residents can bring change to their states' health care systems by indirectly obtaining care for their patients. As EM residents, we are taught to be team leaders in the ED. Should we not expand this role to become leaders in our communities, as well? As physicians invested in providing care to all, we must be proactive in creating a better solution for this large gap in coverage.
REFERENCES
- Cohen LA. Expanding the physician's role in addressing the oral health of adults. American journal of public health. 2013;103:408-12.
- Seu K, Hall KK, Moy E. Emergency Department Visits for Dental-Related Conditions, 2009: Statistical Brief #143. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD)2006.
- McCormick AP, Abubaker AO, Laskin DM, Gonzales MS, Garland S. Reducing the burden of dental patients on the busy hospital emergency department. Journal of oral and maxillofacial surgery: Official journal of the American Association of Oral and Maxillofacial Surgeons. 2013;71:475-8.
- Hocker MB, Villani JJ, Borawski JB, Evans CS, Nelson SM, Gerardo CJ, et al. Dental visits to a North Carolina emergency department: a painful problem. North Carolina Medical Journal. 2012;73:346-51.
- Cohen LA, Bonito AJ, Akin DR, Manski RJ, Macek MD, Edwards RR, et al. Toothache pain: a comparison of visits to physicians, emergency departments and dentists. Journal of the American Dental Association. 2008;139:1205-16.
- Jimenez Y, Bagan JV, Murillo J, Poveda R. Odontogenic infections. Complications. Systemic manifestations. Medicina oral, patologia oral y cirugia bucal. 2004;9 Suppl:143-7; 39-43.
- Edwards PC, Kanjirath P. Recognition and management of common acute conditions of the oral cavity resulting from tooth decay, periodontal disease, and trauma: an update for the family physician. Journal of the American Board of Family Medicine (JABFM). 2010;23:285-94.
- Fox TR, Li J, Stevens S, Tippie T. A performance improvement prescribing guideline reduces opioid prescriptions for emergency department dental pain patients. Annals of emergency medicine. 2013;62:
237-40. - Pajewski NM, Okunseri C. Patterns of dental service utilization following nontraumatic dental condition visits to the emergency department in Wisconsin Medicaid. Journal of public health dentistry. 2012.
- Institute of Medicine (U.S.). Committee on an Oral Health Initiative. Advancing oral health in America. Washington, D.C.: National Academies Press; 2011.
- Cohen LA, Manski RJ, Magder LS, Mullins CD.
Dental visits to hospital emergency departments by adults receiving Medicaid: assessing their use. Journal of the American Dental Association. 2002;133:715-24; quiz 68. - Pettinato ES, Webb MD, Seale NS. A comparison of Medicaid reimbursement for non-definitive pediatric dental treatment in the emergency room versus periodic preventive care. Pediatric dentistry. 2000;22:463-8.
- Nash KD. Geographic Distribution of Dentists in the United States. Retrieved from: www.ada.org/sections/professionalResources/pdfs/topics_economic_geo-2011D.pdf. Date Accessed: Feb 18, 2014.
- Guthrie D, Valachovic RW, Brown LJ. The impact of new dental schools on the dental workforce through 2022. Journal of dental education. 2009;73:1353-60.
- Frisch S. The primary care physician shortage. Bmj. 2013;347:f6559.
- Nash DA. Expanding dental hygiene to include dental therapy: improving access to care for children. Journal of dental hygiene: JDH/American Dental Hygienists' Association. 2009;83:36-44.
- Shoffstall-Cone S, Williard M. Alaska Dental Health Aide Program. International journal of circumpolar health. 2013;72.
- Nash DA, Friedman JW, Mathu-Muju KR, Robinson PG, Satur J, Moffat S, et al. A review of the global literature on dental therapists. Community dentistry and oral epidemiology. 2014;42:1-10.
- ACGME Program Requirements for Graduate Medical Education in Emergency Medicine. Retrieved from: www.acgme.org/acgmeweb/Portals/0/PFAssets/2013-PR-FAQ-PIF/110_emergency_medicine_07012013.pdf. Date Accessed: Feb 18, 2014.