We present a case of arrhythmogenic right ventricular cardiomyopathy (ARVC) with inappropriate implantable cardioverter defibrillator (ICD) discharges triggered by atrial fibrillation (AF) with rapid ventricular response (RVR).
This case underscores the importance of socioeconomic factors in ARVC management and highlights the role of bedside ultrasound, electrocardiographic findings, and multidisciplinary care in guiding treatment.
Clinical History
A 38-year-old male with a history of ARVC s/p dual-chamber ICD placement and paroxysmal atrial fibrillation presented to the emergency department (ED) after three ICD discharges. The patient reported acute left-sided chest pain without syncope, shortness of breath, or systemic symptoms beyond occasional cough and palpitations. He acknowledged poor compliance with his antidysrhythmic medication, sotalol, and anticoagulant, apixaban, due to cost and lack of health insurance.
On exam, he was normotensive, afebrile, saturating 97% on room air, and with irregularly irregular heart rates in the 120-130s. Initial ECG showed atrial fibrillation with RVR and a right bundle branch block (RBBB).
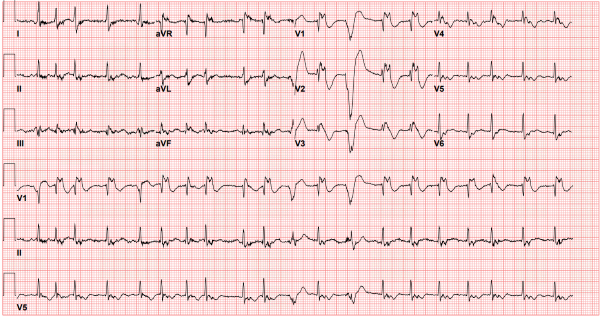
CTA was obtained and showed ground-glass opacities in the right upper lobe suggestive of pneumonia with no pulmonary embolism. POCUS echo showed grossly normal LV systolic function with right ventricular dilation (see Fig 1), and collapsible inferior vena cava (not pictured).
A4C
 PSL
PSL
Discussion
ARVC is an inherited cardiomyopathy characterized by replacement of RV myocardium with fibro-fatty tissue which predisposes patients to ventricular dysrhythmias, progressive RV dysfunction, and sudden cardiac death.1 The ED approach to ARVC necessitates a high index of suspicion, particularly in patients presenting with unexplained syncope, palpitations, or ventricular dysrhythmias. Understanding the underlying pathophysiology, clinical features, and relevant diagnostic tools is critical for timely intervention. Long-term management involves ICD implantation, antidysrhythmic medications, and lifestyle modifications, all of which can be complicated by socioeconomic barriers such as financial constraints and limited access to health care.2
Diagnostic Pearls
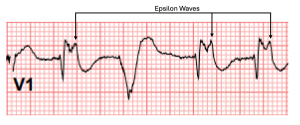
Electrocardiogram: Epsilon wave is the most specific EKG finding in ARVC but is only seen in ~30% of cases. It is characterized by a small deflection at the end of the QRS complex, best seen in leads V1-V2, but may be present in V1-V4. It is caused by pathognomonic myocyte fibrosis leading to delayed depolarization of the RV free wall.4 The most common ECG finding is a prolonged S-wave upstroke ≥ 55 msec in leads V1-V3. Other EKG features include T wave inversions and QRS complex duration >110 msec in leads V1-V3.5
Bedside Ultrasound: Ultrasound findings include disproportionate RV dilation, right atrial enlargement, tricuspid regurgitation, and paradoxical septal bowing of the LV (D-sign).3 In advanced cases decreased tricuspid annular plane systolic excursion (TAPSE <17mm) suggests RV dysfunction. Regional wall motion abnormalities, particularly akinesia or dyskinesia of the RV free wall due to fibro-fatty infiltration, are a hallmark feature.4 These findings, when present in the appropriate clinical context, strongly support the suspicion of ARVC.1
Laboratory Studies
Laboratory evaluations may be helpful in guiding initial management. An elevated troponin level can indicate myocardial injury resulting from dysrhythmia-induced demand ischemia. Assessing electrolyte levels is crucial, as imbalances such as hypokalemia and hypomagnesemia can exacerbate arrhythmic events. Increased brain natriuretic peptide (BNP) levels, although non-specific, can provide insight into the severity of cardiac impairment. Finally, an elevated lactate concentration may signal decreased systemic perfusion and tissue hypoxia, emphasizing the hemodynamic consequences of ARVC.
Rate and Rhythm Control
Patients with ARVC are often adrenergic dependent and are most commonly treated with beta-blockers, in particular sotalol, or amiodarone. Sotalol is a beta-blocker with class III properties that is frequently used in ARVC due to its efficacy in suppressing ventricular dysrhythmias. Other antidysrhythmic medications, including amiodarone and procainamide, can be considered in acute presentations; however, it is important to note that these agents carry a risk of exacerbating dysrhythmias in the fibrofatty RV myocardium. Electrical cardioversion remains first-line for sustained ventricular tachycardia or ventricular fibrillation, while ICD interrogation is critical to deactivate inappropriate shock triggers, optimize device programming, and reduce myocardial injury.4
Hemodynamic Support and RV Failure Management
ARVC-related cardiac dysfunction can precipitate significant hemodynamic instability. Inotropic agents, such as dobutamine or milrinone, may improve RV contractility and reduce afterload, but should be carefully tailored to avoid systemic hypotension and arrhythmogenicity.1 For those with profound instability, vasopressor support with norepinephrine is recommended. Advanced cases may necessitate mechanical circulatory support, including VA-ECMO (Veno-Arterial Extracorporeal Membrane Oxygenation) or pRVADs (percutaneous Right Ventricular Assist Devices), to provide systemic perfusion and unload the RV. Intravenous fluid administration must be judicious in order to optimize RV preload without causing volume overload which leads to further decompensation. Pulmonary vasodilators, including inhaled nitric oxide, may reduce pulmonary vascular resistance, alleviating right-sided heart pressures.
Barriers to Care in the ED
Managing ARVC in the emergency department can be fraught with challenges. The rarity of this condition and its overlap with other arrhythmogenic syndromes can delay diagnosis, especially if key findings like epsilon waves are not present.4 Definitive care often requires electrophysiology and cardiology input, which may be limited in some settings. Emergency physicians must quickly differentiate ARVC-related dysrhythmias, ensure proper rate control, select appropriate antidysrhythmic medications, and treat underlying conditions under time constraints. Access to inpatient resources can facilitate timely multidisciplinary care and lead to improved patient-centered outcomes.2
Case Resolution
ED management began with assessment of the patient's airway, breathing, and circulation, followed by electrolyte repletion, optimization of volume status, and treatment of his atrial fibrillation with RVR with sotalol.1 A chest x-ray showed a left lower lobe infiltrate, so treatment with broad-spectrum antibiotics was initiated for pneumonia which was the likely trigger for his uncontrolled atrial fibrillation.
During hospitalization, the patient underwent a multidisciplinary evaluation to address several critical issues. Electrophysiology confirmed inappropriate ICD discharges, leading to device reprogramming and medication adjustment with an emphasis on cost-effectiveness. Cardiology identified RV dysfunction on echocardiography consistent with ARVC, highlighting the importance of strict rate control and anticoagulation.3 Social work addressed financial barriers by enrolling the patient in an anticoagulation assistance program and coordinating affordable medication access.2 The patient was discharged on day 3 in stable condition with plans for follow-up at a safety-net clinic.
References
- Corrado D, Basso C, Nava A, Thiene G. Arrhythmogenic right ventricular cardiomyopathy: current diagnostic and management strategies. Cardiol Rev. 2001 Sep-Oct;9(5):259-65.
- Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, Quyyumi AA, Taylor HA, Gulati M, Harold JG, Mieres JH, Ferdinand KC, Mensah GA, Sperling LS. Socioeconomic Status and Cardiovascular Outcomes: Challenges and Interventions. Circulation. 2018 May 15;137(20):2166-2178.
- Yoerger DM, Marcus F, Sherrill D, et al. Multidisciplinary Study of Right Ventricular Dysplasia Investigators. Echocardiographic findings in patients meeting task force criteria for arrhythmogenic right ventricular dysplasia: New insights from the multidisciplinary study of right ventricular dysplasia. J Am Coll Cardiol. 2005;45(6):860-865.
- Marcus FI, McKenna WJ, Sherrill D, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the Task Force Criteria. Eur Heart J. 2010 Apr;31(7):806-14.
- Yoerger DM, Marcus F, Sherrill D, Calkins H, Towbin JA, Zareba W, Picard MH; Multidisciplinary Study of Right Ventricular Dysplasia Investigators. Echocardiographic findings in patients meeting task force criteria for arrhythmogenic right ventricular dysplasia: new insights from the multidisciplinary study of right ventricular dysplasia. J Am Coll Cardiol. 2005 Mar 15;45(6):860-865.
Fig 1. Point-of-Care Ultrasound: Apical 4 chamber and parasternal long views show grossly normal left ventricular systolic function and right ventricular (RV) dilation (collapsible inferior vena cava not pictured).