INTRODUCTION
Stroke remains a major cause of morbidity and mortality worldwide, with hemorrhagic strokes accounting for approximately 10–20% of cases.¹ Classic symptoms like hemiparesis or aphasia often lead to early recognition, but atypical presentations—such as isolated wrist drop—can delay diagnosis. These are frequently misattributed to peripheral nerve injuries such as radial neuropathy or brachial plexus lesions.2,3
The “hand knob” region of the precentral gyrus, which controls hand and finger movement, has been implicated in rare cases of isolated upper limb weakness. Most hand knob strokes are ischemic, with only a small proportion being hemorrhagic.4-6 One study found that hand knob strokes accounted for just 0.9% of all strokes, with 10.5% of those being hemorrhagic.6 These cases often lack systemic findings, complicating recognition in the emergency setting.
We present a rare case of isolated left wrist drop caused by a hemorrhagic stroke localized to the hand knob. To our knowledge, there is no published hemorrhagic stroke “hand-knob” stroke published in the emergency medicine literature.
CASE REPORT
A 50-year-old male construction worker presented with a 4-day history of sudden-onset left wrist weakness. He denied trauma, compression, or recent alcohol use. His history included 30 years of daily heavy alcohol intake (six 16-ounce malt liquors) and a 25-year smoking history. He had no known hypertension, diabetes, or other chronic illness.
On exam, he was alert and hemodynamically stable. Neurologic assessment revealed isolated left wrist drop with 0/5 strength in wrist and finger extension, flexion, and abduction. Sensation was decreased distal to the wrist. The limb was cool with delayed capillary refill, though a +2 radial pulse was present. Cranial nerves were intact, and no other focal deficits were noted.
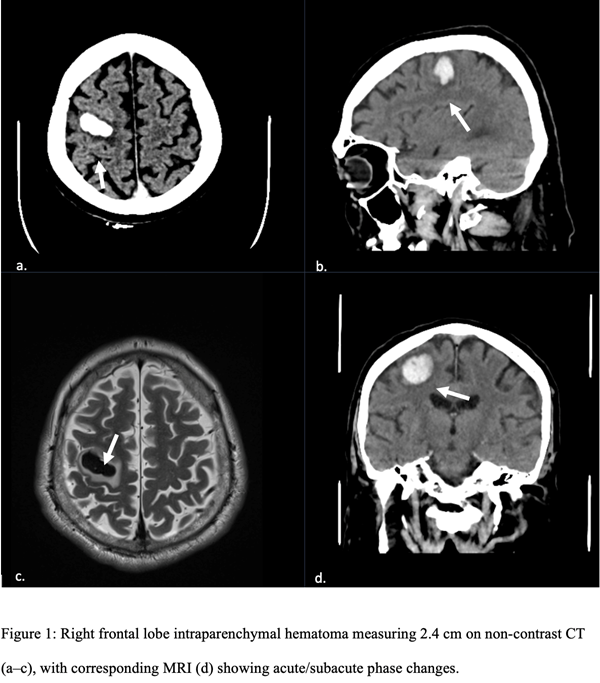
Chest X-ray and upper extremity Doppler studies were unremarkable. A non-contrast head computed tomography (CT) revealed a right frontal intraparenchymal hemorrhage measuring 2.5 × 1.2 cm with mild edema but no midline shift (Figure 1). Magnetic resonance imaging (MRI) confirmed the lesion in the hand knob region and excluded vascular malformations.
He was admitted to the neurocritical care unit for blood pressure control and alcohol withdrawal prophylaxis using thiamine and folate. Neurosurgery and neurology co-managed the case. No surgical intervention was required. With supportive care and physical and occupational therapy, he improved and regained full strength and sensation in his left upper extremity, including his hand and wrist, and was discharged with outpatient follow-up.
DISCUSSION
This case highlights a diagnostic pitfall in emergency medicine—assuming all wrist drop is peripheral. The hand knob region, a distinct cortical area, is rarely affected in isolation, and hemorrhagic variants are even more uncommon.4-6 In Zhang et al.’s series, only 10.5% of hand knob strokes were hemorrhagic.⁶
To our knowledge, there are no published cases in the emergency medicine literature describing a hemorrhagic stroke of the hand knob region presenting solely as isolated wrist drop. This absence underscores the need for emergency physicians to consider cortical etiologies, even when classic stroke features are lacking.
In this patient, chronic alcohol use—associated with hypertensive spikes, coagulopathy, and nutritional deficiencies—was the likely contributor.2 There were no traditional vascular risk factors, and the presentation mimicked peripheral neuropathy.
Timely imaging was key. Anchoring bias could have delayed diagnosis and appropriate management. Multidisciplinary involvement facilitated non-operative care and effective recovery.
Key takeaways for emergency medicine practice include:
- Atypical presentations of stroke, such as isolated wrist drop, require a high index of suspicion and early imaging to exclude central causes.
- Chronic alcohol use should raise concern for hemorrhagic stroke and prompt a comprehensive evaluation for systemic and neurologic complications.
- Coordinated, multidisciplinary care is essential for optimal recovery and avoidance of unnecessary interventions.
CONCLUSION
This case highlights the diagnostic complexities of hemorrhagic stroke presenting with isolated wrist drop. Emergency physicians should maintain a high index of suspicion for central nervous system causes in patients with unexplained peripheral motor deficits. Early imaging and a multidisciplinary approach are essential for optimizing patient outcomes. Enhanced public health efforts are needed to improve awareness and prevention of stroke in high-risk populations.
REFERENCES
- Caplan LR. Intracerebral hemorrhage: A review. Lancet Neurol. 2020;19(10):800-812.
- Greenberg SM, Altschul D, Anderson CS, et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage. Stroke. 2022;53(6):e282-e361.
- Vagal A, Wintermark M, Nael K, et al. Automated CT perfusion imaging for stroke. Neurology. 2019;93(9):888-898.
- Finkelsteyn AM, Saucedo MA, Miquelini LA, et al. Ischemic stroke of the “hand knob area”: A case series and literature review. J Clin Neurosci. 2019;65:100-105.
- Hussain SHZ, Kiani I, Ali A, Zeeshan A, Khalid H, Mahmood F. Cortical hand knob stroke: a case report of isolated hand palsy with a review of the literature. Cureus. 2024;16(5):e73840.
- Zhang Z, Sun XX, Liu X, Wang L, Zhu R. Clinical features, etiology, and prognosis of hand knob stroke: a case series. BMC Neurol. 2022;22(1):348.
Funding/Support:
The authors received no external funding for this case report.
Conflict of Interest Disclosures:
The authors report no conflicts of interest.
Acknowledgments:
None.
Author Contributions:
Mr. Contreras and Ms. Han drafted the original version of the case report. Dr. Rincon reviewed and edited multiple drafts. Dr. Khan contributed to revisions and obtained the clinical images. Dr. Brown provided final editorial oversight. All authors reviewed and approved the final manuscript.
Informed Consent:
Written informed consent was obtained from the patient for publication of this case report and accompanying images.