Gastrointestinal bleeding has classically been divided into upper and lower GI bleeds based on the location of the bleed in relation to the ligament of Treitz.
Lower GI bleeding is less common.1,2 Diverticulosis, hemorrhoids, neoplasm, and ischemic bleeding are the most common causes.1 In-hospital mortality is relatively low (3.9%) when compared to upper GI bleeding.3 Mortality is worse in older patients, those with comorbidities, coagulopathy, anticoagulation use, and bowel ischemia. Lower GI bleeds are typically treated medically and with angiography, colonoscopy, or surgery.3 Balloon tamponade devices specifically designed for upper GI bleeding are well established as a temporizing measure in life-threatening upper gastrointestinal bleeding, but rarely have been used for lower GI bleeding.
CASE
A 58-year-old male with a past medical history of metastatic colon cancer status post subtotal colectomy with ileostomy, chemotherapy, radiation, and immunotherapy presented to the ED with bright red rectal bleeding and bloody output from his ostomy bag. He was found to be tachycardic and hypotensive with a hemoglobin of 7.1 g/dL. CT angiography of the abdomen and pelvis showed a necrotic rectal mass. Surgery was consulted but no operative management was pursued. He was transfused a total of 3 units of packed red blood cells and then admitted to the MICU. Due to a bed shortage the patient boarded in the ED overnight. He was transfused an additional 2u PRBCs and FFP during that time.
The next afternoon emergency physicians were called emergently to the patient’s room for a change in clinical status. He was found with clothes soaked in blood and a copious amount of blood pooled in the hospital bed, with systolic blood pressures in the 50s. An emergent femoral venous introducer was placed, and massive transfusion protocol was initiated. Examination of the rectum revealed a large amount of blood with evident arterial pulsations against the examiner’s finger interior to the anal sphincter. External and internal direct pressure along with gauze packing soaked in tranexamic acid were attempted but the patient continued to exsanguinate bright red blood from his rectum. Despite multiple units of PRBCs, FFP and platelets systolic blood pressure remained in the 50s-60s. At that point, the decision was made to take more aggressive measures to control bleeding. Physicians from surgery, gastroenterology, MICU, and interventional radiology were at bedside. Surgical services confirmed the patient had approximately 11 inches of blind rectal pouch.
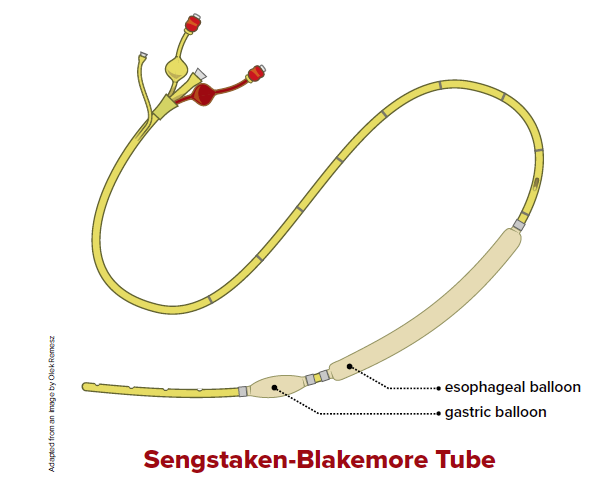
In an attempt to tamponade the arterial bleeding at or near the anal ring, a Sengstaken-Blakemore tube was inserted into the patient's rectum until the esophageal balloon was completely into the rectum past the anal sphincter. The distal gastric balloon was not inflated due to concern for ischemic necrosis and perforation of the rectal vault from overdistention. The esophageal balloon was inflated with 40cc of air and drainage port clamped.
The initial hope was direct tamponade of the bleeding site. However, profuse bleeding continued. The balloon was repositioned so that proximal end of the esophageal balloon protruded from the anus, with the intent of either directly tamponade of bleeding, or occluding the exit of blood so that the closed space would eventually fill with blood and cause tamponade itself.
Upon re-inflation of the balloon SBPs rapidly improved to the 80s and then the 90s. There was no further active bleeding evident. The patient tolerated the procedure without complaint, stating the tube was not causing significant discomfort. He was taken emergently by IR for embolization and coiling of a left internal iliac artery pseudoaneurysm that communicated with his necrotic rectal mass. After the procedure, the patient was taken to the MICU.
During his admission he received a total of 15u PRBCs, 8 units FFP and 3 units platelets before being discharged to hospice. At the patient’s insistence, the Sengstaken-Blakemore tube was left in place at discharge.
Discussion
Literature review shows only a few cases where balloon tamponade devices intended for upper gastrointestinal bleeding were used for lower GI bleeding.4-10 Each of these involved life-threatening bleeding that was not stopped by traditional methods. In this case, rectal insertion of the Blakemore tube with repositioning to include the anal ring temporarily stabilized an otherwise exsanguinating patient, bridging them to definitive treatment. This case is unique in that the patient left the hospital with the device in place. Here we highlight the utility of balloon tamponade as a temporizing measure for life-threatening lower GI bleeding when more traditional means fail.
References
- Ghassemi KA, Jensen DM. Lower GI bleeding: epidemiology and management. Curr Gastroenterol Rep. 2013 Jul;15(7):333.
- Wuerth BA, Rockey DC. Changing Epidemiology of Upper Gastrointestinal Hemorrhage in the Last Decade: A Nationwide Analysis. Dig Dis Sci. 2018 May;63(5):1286-1293.
- Strate LL, Ayanian JZ, Kotler G, Syngal S. Risk factors for mortality in lower intestinal bleeding. Clin Gastroenterol Hepatol. 2008 Sep;6(9):1004-10; quiz 955-.
- McGuinness J., Winter D.C., O’Connell P.R. Balloon tamponade to control haemorrhage following transanal rectal surgery. J. Colorectal Dis. 2004;19:395–396
- Cho S.M., Al-Khafaji A., Ahmad J. Minnesota tube for bleeding rectal varices. J. Gastroenterol. 2006;101:S284–285.
- Marshall B.J., Seow C.H., Levitt M.D. Use of a Minnesota tube to tamponade bleeding from an ileorectal anastomosis. ANZ J. Surg. 2007;77:916–917.
- Neeki M.M., Raj V., Archambeau B., Arabian S., Hussain F. Novel application of balloon tamponade in management of acute lower gastrointestinal hemorrhage. Pract. Cases Emerg. Med. 2019;3:243–247.
- Roy M.K., Rhodes M., Ruttley M.S., Wheeler M.H. Sengstaken tube for bleeding rectal angiodysplasia. J. Surg. 1996;83:1111.
- Michopoulou A.T., Doulgerakis G.E., Pierrakakis S.K. Sengstaken-Blakemore tube for massive haemorrhage following rectal biopsies. J. Colorectal Dis. 2013;28:1595–1596.
- Fadel MG, Boshier PR, Howell AM, Iskandarani M, Tekkis P, Kontovounisios C. The management of acute lower gastrointestinal bleeding using a Sengstaken-Blakemore tube. Int J Surg Case Rep. 2020;75:394-397.