ARTICLE
Scott JH, Gordon M, Vender R, et al. Venoarterial Extracorporeal Membrane Oxygenation in Massive Pulmonary Embolism-Related Cardiac Arrest: A Systematic Review. Crit Care Med. 2021;49(5):760-769.
BACKGROUND
Massive pulmonary emboli (PE) -- which are pulmonary emboli that induce sustained hypotension, pulselessness, or sustained bradycardia -- are incredibly deadly, even with intervention.3-5 For those patients with massive PE who subsequently arrest, data suggests mortality as high as 90%.
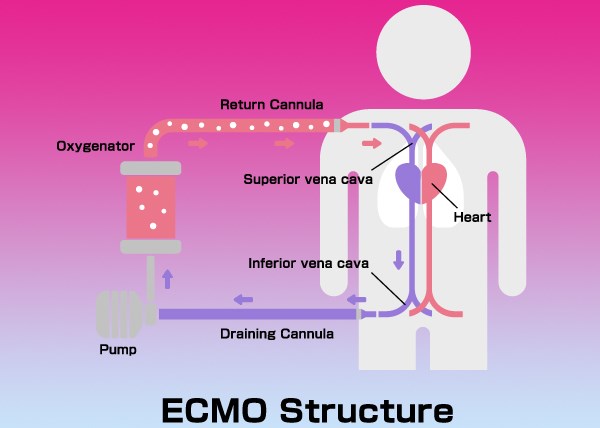
One avenue of potential treatment in massive PE is the use of Extracorporeal Membrane Oxygenation, commonly known as ECMO. ECMO comes in two major forms, veno-arterial (VA) and veno-venous (VV). In brief, VA-ECMO provides both hemodynamic and respiratory support by offloading the responsibility for circulation from heart and oxygenation by the lungs. In the setting of PE, this allows time for acute treatment (such as thrombolysis or embolectomy) to work in addition to long term benefits (such as return of right ventricular function). Conversely, VV-ECMO provides primarily respiratory support, offloading the responsibility of oxygenation from the lungs, while still relying on the heart for circulatory function, and is not commonly used in PE treatment. As the use of ECMO becomes more available at increasing numbers of institutions, questions about the logistics of VA-ECMO in PE remain, particularly regarding patient characteristics, the timing of cannulation relative to CPR, and of the administration of thrombolytics, given the risk of arterial bleed.
OBJECTIVE
To review the literature which has previously reported on survival and the predictors of mortality in patients with massive PE in cardiac arrest who received VA-ECMO.
DESIGN
A systematic review developed for PubMed and translated for Embase, Cochrane Central, Cinahl, and Web of Science using related terms to the topic.
STUDY SELECTION
A total of 1,374 studies were identified. Duplicates were excluded and remaining abstracts were screened by two independent reviewers, with a third as tie-breaker. This process was repeated for full-text articles. The statistical significance of findings was determined with unpaired t tests for continuous variables and with chi-square tests for categorical variables. Logistic regression models were performed to derive the unadjusted or adjusted odds ratio (OR) of mortality.
Studies that met inclusion criteria:
- Described very specific clinical scenario of massive PE with cardiac arrest managed with VA-ECMO
Primary outcome
- Survival to discharge
Secondary outcomes
- Impact of age
- Systemic thrombolysis before ECMO
- ECMO cannulation during CPR or after return of spontaneous circulation (ROSC)
- PE as the primary reason for admission
- Hospital location of ECMO cannulation on mortality
- Occurrence rate of major bleeding
KEY RESULTS
A total of 77 studies were included with a total of 301 patients
Primary Outcome
- 183 patients (61%) survived to discharge
Selected Secondary Outcomes
- Patients older than 65 years old had a greater risk of death (OR 3.56, p =0.02)
- Cannulation during CPR increased risk of death compared to after ROSC (OR 6.45, p=0.01)
- 51 patients received systemic thrombolysis prior to VA-ECMO (17% of total 301 patients)
- 34 survived to discharge (67%)
- No increased risk of death in these patients (OR 0.78, p =0.48)
- 6 patients had a major bleeding event; all 6 survived
- There was no difference in survival between PE and non-PE admissions or where in the hospital the cannulation occured (ED, cardiac catheterization lab, ICU, OR, medical/surgical floor)
- Of those reporting bleeding events (21) there was a 76% survival rate and of those reporting no major bleeding event (30), there was an 80% survival rate
STRENGTHS
- First systematic review of VA-ECMO in massive PE-related cardiac arrest
- Included gray literature through clinicaltrials.gov and preprints
- Able to provide answers to primary and multiple secondary outcomes
LIMITATIONS
- Only 7% of patients in this study had a major bleeding event which is not consistent with previous studies which have reported 40-54%1,2
- Multiple variables were unknown for certain patients including age, gender, primary reason for admission, location in hospital cannulation was performed, if thrombolysis was received, or timing of cannulation in cardiopulmonary resuscitation
- Literature review inherently has limitations in data and consistency and should not be compared to the highest-level of evidence: an RCT
EM TAKE-AWAYS
The data and support for VA-ECMO for cardiac arrest after massive PE is still lacking, but if your institution has the resource, consider VA-ECMO. According to this systematic review, of all patients who received VA-ECMO during cardiac arrest, those older than 65 and those who were cannulated during CPR had increased mortality. While this review reported a low bleeding risk, previous studies have reported significantly higher rates of bleeding and providers should be prepared for the consequences of cannulating after thrombolysis.6
REFERENCES
- Al-Bawardy R, Rosenfield K, Borges J, et al. Extracorporeal membrane oxygenation in acute massive pulmonary embolism: A case series and review of the literature. Perfusion. 2019; 34:22–28
- Cheng R, Hachamovitch R, Kittleson M, et al. Complications of extracorporeal membrane oxygenation for treatment of cardiogenic shock and cardiac arrest: A meta-analysis of 1,866 adult patients. Ann Thorac Surg. 2014;97(2):610–616.
- Jaff MR, McMurtry MS, Archer SL, et al. Management of Massive and Submassive Pulmonary Embolism, Iliofemoral Deep Vein Thrombosis, and Chronic Thromboembolic Pulmonary Hypertension. Circulation. 2011;123(16):1788–1830.
- Stulz P, Schlapfer R, Feer R, Habicht J, Gradel E. Decision making in the surgical treatment of massive pulmonary embolism. Eur J Cardiothorac Surg. 1994;8(4):188–193.
- Kucher N, Rossi E, DeRosa M, Goldhaber SZ. Massive pulmonary embolism. Circulation. 2006;113:577-582.
- Oh YN, Oh DK, Koh Y, et al. Use of Extracorporeal Membrane Oxygenation in Patients with Acute High-Risk Pulmonary Embolism: A Case Series with Literature Review. Acute Crit Care. 2019;34(2):148-154.