A 44-year-old male with a past medical history of substance use disorder presented to the emergency department following an overdose. The patient was reported to have taken 1 gram of heroin and 22 mg of illicitly purchased “Xanax” orally in an effort to avoid police detection.
EMS noted that he was initially alert on scene but became somnolent en route. He was given 8 mg IN naloxone prior to arrival to the ED with no clinical improvement. He was subsequently given an additional 4 mg IV naloxone in the emergency department when he arrived. Despite this, he remained obtunded with minimal respiratory effect and was intubated for airway protection.
In the ED, on telemetry the patient was noted to be developing bradyarrhythmias. An initial EKG was performed and was notable for bradycardia with multiple PVCs of variable morphology, including ventricular couplets (Figure 1). Telemetry continued to show dynamic changes in his rhythm remaining bradycardic with HR 40-50s; therefore, an EKG was repeated within minutes, this time showing ventricular bigeminy (Figure 2).
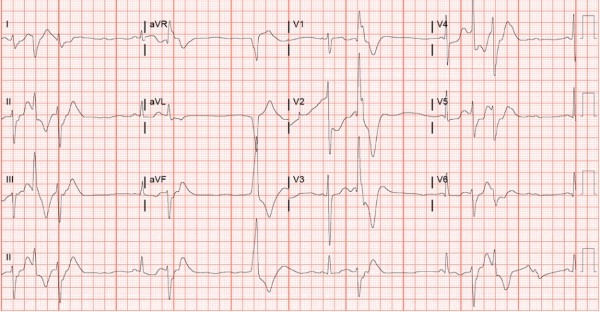
Figure 1
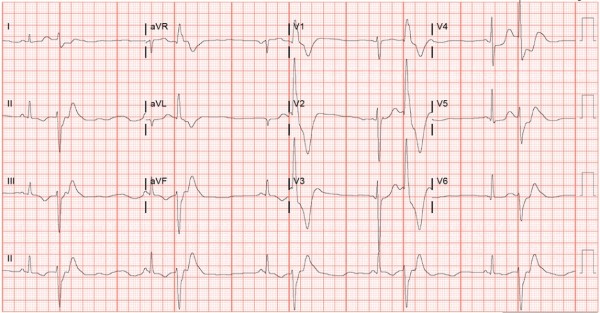
Figure 2
The patient was admitted to the ICU for continued management. Four hours after admission, his EKG showed bradycardia with QTc prolonged to 648 (Figure 3). Due to his unique presentation, an extended toxicology panel of testing was ordered to investigate contaminants with possible cardiac effects.
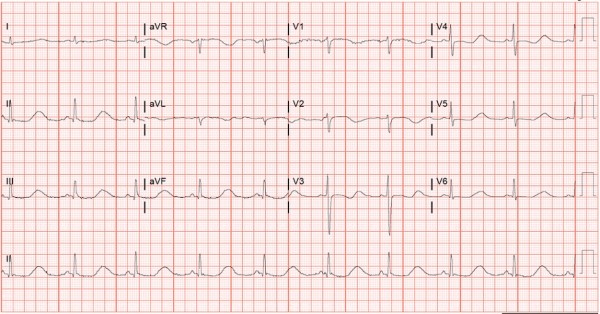
Figure 3
The patient was found to have a quantitative etizolam level of 160 ng/mL and its major metabolite alpha-hydroxyetizolam (at 100 ng/mL). No other tested novel psychoactive substances — including a large number of illicitly manufactured fentanyls (IMF) — were detected. The patient had intermittent episodes of bradycardia following his overdose that resolved by hospital day 3. QTc remained >600 for several days but was 460 by the second week of his stay. On the last day of his hospital stay, his EKG was normal sinus rhythm with a rate in the 70s and normalized QTc.
Discussion
Etizolam is an illicit benzodiazepine, not medically approved in the United States. To our knowledge, no novel illicit benzodiazepine has been associated with bradycardic dysrhythmias.
Studies have shown that the use of novel psychoactive substances, including illicit benzodiazepines, has been on the rise in the United States.1 According to the National Poison Data System, there was a 330% increase in incidence from 2014 to 2017, and this trend has likely continued.2 Although the use of illicit benzodiazepines is rising, users may not know they are taking them. Illicit benzodiazepines have been reported in candy-like pills, and other times users (like the patient in our case) may think they are buying a different drug.
Benzodiazepines can now be found for sale online without restrictions.4 The FDA Office of Criminal Investigation reported 130 criminal action cases against counterfeiting organizations from 2016 to 2021. Of these cases, 64.6% involved products being sold online, and in 84.6% of cases, the counterfeit medications could be obtained without a prescription. The counterfeit medications identified in these cases were most frequently in the sexual dysfunction, opioid, stimulant, anabolic steroid, and benzodiazepine drug classes. The counterfeit benzodiazepines were found to include non–FDA-approved active ingredients with different pharmacokinetics. The medications sold often had inconsistencies in the dosage of active ingredients from pill to pill. These factors significantly raise the risk of respiratory depression and accidental overdose when compared with FDA-approved versions of these medications. There are more than 50,000 online pharmacies, and 80% of all rogue web-based pharmacies target English-speaking countries.5
Recognizing illicit benzodiazepine overdose is challenging for the emergency physician because these substances often are not identified on routine drug screening, and clinicians must rely on patients to self-report use. Such substancescan be identified on lab-based testing; however, that process does not produce information quickly enough to help in the acute setting and requires a level of suspicion to pursue.3
Emergency physicians are very familiar with benzodiazepines and may encounter frequent cases involving patient use, but the novel substances introduce a myriad of unknowns. While illicit benzodiazepines are structurally derived from medically approved benzodiazepines, they are not medically licensed and likely have symptoms and effects that still need to be classified. Our case is an example of potential cardiac effects.
Conclusion
Recent literature shows that illicit benzodiazepines have been associated with significant impairment, have higher potencies than standard benzodiazepines, and are harder to identify via screening methods routinely used for standard benzodiazepines.1 Novel illicit benzodiazepines are becoming a contaminant of concern, both alone and in combination with opioids.
Further research must be conducted on novel illicit benzodiazepines. Until more is known about these substances, it is important to monitor their prevalence and update data routinely, as they have already proven to be a threat to public safety.
References
- Edinoff AN, Nix CA, Odisho AS, Babin CP, Derouen AG, Lutfallah SC, Cornett EM, Murnane KS, Kaye AM, Kaye AD. Novel Designer Benzodiazepines: Comprehensive Review of Evolving Clinical and Adverse Effects. Neurol Int. 2022 Aug 22;14(3):648-663
- Carpenter J.E., Murray B.P., Dunkley C., Kazzi Z.N., Gittinger M.H. Designer benzodiazepines: A report of exposures recorded in the National Poison Data System, 2014–2017. Clin. Toxicol. 2019;57:282–286.
- Heide G., Høiseth G., Middelkoop G., Øiestad Å.M.L. Blood Concentrations of Designer Benzodiazepines: Relation to Impairment and Findings in Forensic Cases. J. Anal. Toxicol. 2020;44:905–914
- Pope J.D., Weng Choy K., Drummer O.H., Schneider H.G. Novel Benzodiazepines (Clonazolam and Flubromazolam) Identified in Candy-Like Pills. J. Appl. Lab. Med. 2018;3:48–55.
- White C.M. Criminal Action Against Drug Counterfeiters: Assessment of the FDA Office of Criminal Investigation Database 2016 Through 2021. Ann Phamacother. 2022. 56(12) 1333-1338.



