Ventilators, Alarms, and You
You are caring for a patient who arrived in acute respiratory failure requiring rapid sequence intubation. Establishing the airway itself was not problematic and no airway abnormalities were seen during intubation. After stabilizing the patient, you step out of the room to tend to another ill patient.
Some time later, the nurse from your first patient notifies you that the ventilator alarms keep going off, and that respiratory therapy is busy caring for another critically ill patient. Being the centered and disciplined resident that you are, you step into the room to begin systematically evaluating the situation.
What is your first move?
The goal of this article will be to review the basic concepts of volume and pressure characteristics in mechanically ventilated patient so that you will be able to interpret variations that trigger alarms. After reviewing the fundamentals, the article will review common causes of triggered ventilator alarms and how to troubleshoot these issues.
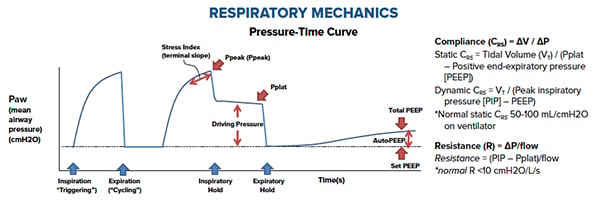
Interpreting the Pressure-Time Curve
While you may notice several waveforms on the ventilator, each with their own nuances, a fundamental understanding of the pressure-time curve is important for the emergency physician. Pressure is created when there is flow directed into a closed system, such as the lungs. Resistance is created in this system from the Endotracheal tube (ETT), the airway, the chest wall, and the lung itself. Generally, there are 2 pressures that we need to be familiar with to understand this.
Peak Pressure (Ppeak): This is the summation of pressure generated by the ventilator to overcome airway (ETT and bronchus) resistance and alveolar resistance to attain peak inspiratory flow and to deliver desired tidal volume.
Put simply, it is the amount of airway pressure delivered by the ventilator to initially overcome the resistance of the ETT, airway, and alveoli. As you may recall from your undergraduate physics courses, resistance to flow is inversely proportional to radius (see Poiseuille’s Law). Peak pressure is graphed as a summation of both initial airway resistance and lung compliance. In general, an acceptable maximum Ppeak is 40 cmH2O.
Plateau Pressure (Pplat): Plateau pressure is the pressure in the lung after a certain volume is delivered into the lungs. This is measured by doing an inspiratory hold, which effectively eliminates any airway resistance (when flow stops, resistive work is zero) from the equation. This is a gross reflection of lung compliance, or “stiffness.” Given the absence of flow when measuring the plateau pressure, the main determinant of plateau pressure is compliance. This may be easier to understand if you think that they are inversely proportional: if lungs are very compliant or "stretchy" then the resultant plateau pressure reflected will be lower. The opposite is true of stiff lungs, or low compliance.
So what is compliance really? Compliance is simply the change in volume divided by the change in pressure; if you have a large change in volume with low-pressure change, compliance will be high. Compliance plays a role in both calculating Ppeak and Pplat. In general, an acceptable maximum Pplat is 30 cmH2O. Changes in airway resistance and compliance can affect the pressure-time curve.
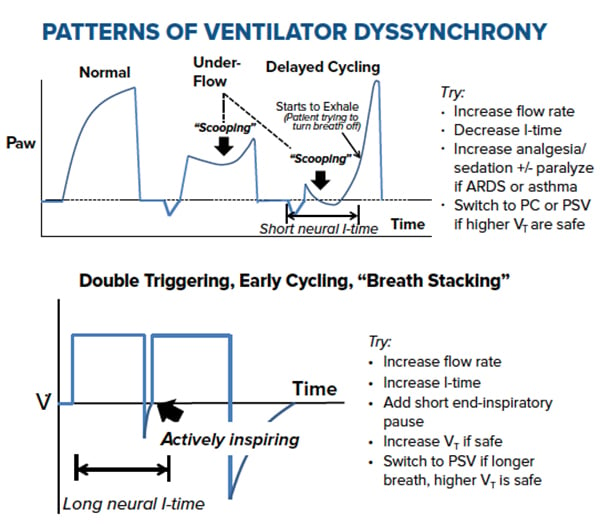
Troubleshooting Alarm Types: Moving Beyond DOPES
During ventilator troubleshooting, many residents are taught the DOPES mnemonic: check for Dislodgement, Obstruction of the ETT from mucus plugs or from patients biting on the tube, Pneumothorax, Equipment malfunction, and Stacked Breaths or patient ventilator dyssynchrony. The goal of this section is to move beyond DOPES and thereby gain an understanding of the different alarm types, their associated waveforms, and the etiologies triggering the alarms. While different ventilators will use different displays or alarm configurations, the below concepts hold true regardless of model.
1. Low Peak Pressure: Think Air Leak
The ventilator alarm is alerting you “low peak pressure” (or simply “low pressure”). There is a leak in the system and the ventilator is not able to generate the peak or plateau pressure necessary to oxygenate or ventilate the patient.
ETT Position Too High: Check ETT depth: is it in the same position as during initial intubation? Dislodged during transport? Consider repeating a chest x-ray.
ETT Cuff Leak: Some ventilators will show and adjust cuff pressure on the monitor. Cuff pressure may need to be increased or the entire ETT replaced. Also consider a leak in the ETT/ventilator interface as well as the tubing connecting the ventilator to the ETT.
Take-Home Points
Chest Tube Leak: Confirm distal chest tube holes are in the pleural space and that there are no leaks in the tubing or connections. Consider repeating a chest x-ray and advancing the tube as needed.
Bronchopulmonary Fistula: Rare cause but consider in patients with a history of tuberculosis, radiation therapy, chemotherapy, or who have undergone lung resections. This etiology is ultimately diagnosed via bronchoscopy.
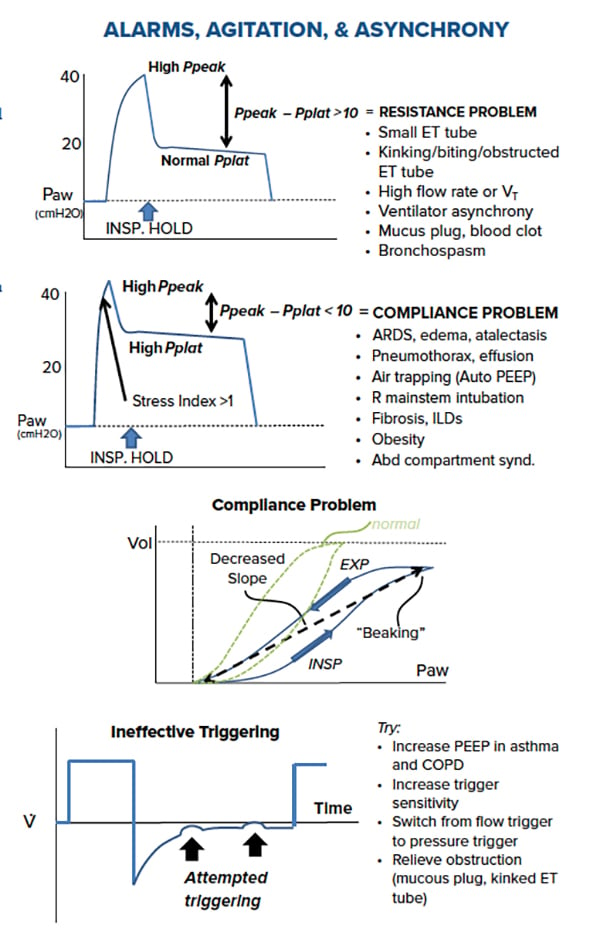
2. High Peak Pressure, Normal Plateau Pressure: Think Resistance
The ventilator is showing isolated high peak pressures. There is resistance in the ETT or distal bronchus causing a smaller diameter and requiring the ventilator to increase pressure in order to deliver the same breath. When taken off the ventilator, these patients will have increased resistance with manual ventilation.
Bronchospasm: Does the patient’s history or exam indicate reactive airway disease or anaphylaxis? Consider a trial of bronchodilators, steroids, or epinephrine.Obstruction in the ETT: Consider a mucous plug (improved with frequent Chest PT, in-line suctioning, bronchoscopy), aspiration event (is the ETT cuff pressure adequate?), hemoptysis (traumatic from ETT placement?), or possible water or condensation in ventilator circuit or the heat exchanger.
Kink in the Circuit: Consider ventilator tubing kink or is the patient biting the tube?
Consider bite block and proper sedation and analgesia.
ETT size: Is this the right size ETT for your patient? This can often be an issue in pediatrics.
3. High Peak Pressure, High Plateau Pressure: Think Compliance
The ventilator is showing high peak and plateau pressures. There is an issue with the compliance of the lungs requiring the ventilator to increase the pressure delivered. These are the most common types of ventilator alarms.
Evolving Pneumonia: Consider Ventilator-Associated Pneumonia; this can be indicated by a new-onset increase in FiO2 or PEEP requirement. Repeat a chest x-ray or look for increase in sputum, fevers, or leukocytosis.
Pulmonary Edema: Can be caused by congestive heart failure, ARDS, increased overall volume status, or sudden catecholamine-release (“Flash Pulmonary Edema”). Consider diuretics, condensing IV fluids given, and adjusting PEEP.
Auto-PEEP: Caused by breath stacking in patient with progressively increasing PEEP and often seen in patients with obstructive sleep apnea, COPD, and reactive airway diseases. This may be caused by inappropriate PEEP levels, tidal volumes, or ventilator dyssynchrony (consider sedation and analgesia). This can be immediately improved by removing patient from the ventilator and manual ventilation. Left unchecked, this can cause hypotension and barotrauma. Consider adjusting the respiratory rate, tidal volume, and/or inspiratory/expiratory ratio.
Right Mainstem Intubation: Check ETT depth, bilateral breath sounds, chest x-ray and adjust accordingly.Tension Pneumothorax: Can be caused by barotrauma or volutrauma. Watch for hypotension and consider immediately disconnecting the patient from the ventilator and emergent decompression with thoracostomy. Positive pressure ventilation by exacerbate a previously unnoticed pleural leak.Miscellaneous: Once the above causes have been ruled out, consider other causes such as atelectasis, pulmonary fibrosis, abdominal distension (ileus, diaphragm injury), or circumferential burns.
4. Hypoxia without Change in Ventilator Curve: Think Shunt
This is generally caused by dead-space ventilation or poor perfusion. Consider an intracardiac shunt (ie, PFO), pulmonary embolism, AV-fistula, hypovolemia, and shock states.
- Ventilator alarms are a common occurrence both in post-intubation and chronic ICU patients. Alarms can be the first sign of an acute process and should be addressed immediately.
- Assessment of the Pressure-Time Curve, Ppeak, and Pplateau will help differentiate different causes of ventilator alarms. Physical exam findings, checking ETT placement, and repeating a chest x-ray can also be key to diagnosing causes. When initially unsure, refer to the DOPES mnemonic.
- When in doubt, take the patient off the ventilator and manually ventilate. If the patient gets better, it’s likely the ventilator, the interface, or the settings. If the patient does not get better, consider an issue with the patient or with the ETT.