A 30-year-old male with a history of hypertension presented to the ED with a foreign body sensation in his throat.
He denied eating anything recently and did not recall something that may have gotten stuck. He was swallowing well and tolerating secretions. He stated that he tried carbonated drinks and water, but nothing alleviated his symptoms. He also reported an occasional burning sensation. His vitals on arrival were: HR 65; RR 16; temp 36.7C; BP 197/136; andO2 100%.
Physical examination revealed a patient whose airway was patent with no pooling of secretions or stridor. Oropharynx was non-erythematous without signs of uvular deviation or peritonsillar abscess. No masses or swelling palpated in the submandibular space or around the neck.
Soft tissue neck radiograph was ordered to evaluate for potential foreign body and demonstrated a calcified stylohyoid ligament. This is associated with a foreign body sensation called Eagle’s Syndrome.
Discussion
Eagle’s Syndrome was described by otolaryngologist Dr. Watt W. Eagle in 1937. It is characterized by calcified stylohyoid ligament or an elongated styloid process. The average length of the styloid process varies between 20mm and 30mm in adult Caucasians, and between 15.4mm and 18.8mm in the Asian population.4 Some estimates suggest that approximately 4-7% of the general population have elongated styloid processes, with about 4-10% of them being symptomatic.1 This process can occur bilaterally or unilaterally. Females have an increased likelihood of presenting with Eagle’s Syndrome, and it is more common among patients older than 50 years. It can also be seen in patients after throat trauma or tonsillectomy.
The causes of elongation are unclear, but include: 1) congenital elongation, 2) calcification of stylohyoid ligament due to an unknown process or associated with conditions increasing heterotopic calcification, such as in disorders of calcium or phosphorous metabolism or patients with chronic renal failure, or 3) growth of osseous tissue at the insertion point of the stylohyoid ligament.3
Eagle initially described two types of syndromes: 1) classic styloid and 2) carotid artery. The former is associated with cranial nerve impingements related to compression of CN V, VII, IX, X. This was more commonly described after tonsillectomy as a result of fibrous tissue distorting nerve fibers in the tonsillar fossa. The latter is associated with vascular or ischemic pain as well as sympathetic plexus irritation, and was not associated with tonsillectomy.2
As mentioned above, presentation of Eagle’s Syndrome can range in symptomatology. Some described symptoms include difficulty swallowing, foreign body sensation, craniofacial pain from neurovascular irritation, pain on neck rotation, hypersalivation, voice changes, otalgia, tinnitus, and headache or dizziness if the carotid artery is compressed.5 Furthermore, compression of perivascular sympathetic fibers may lead to a presentation of Horner Syndrome. As these symptoms are nonspecific and may mimic other clinical presentations, it is important to rule out life-threatening etiologies and consider other causes and assess for airway compromise.
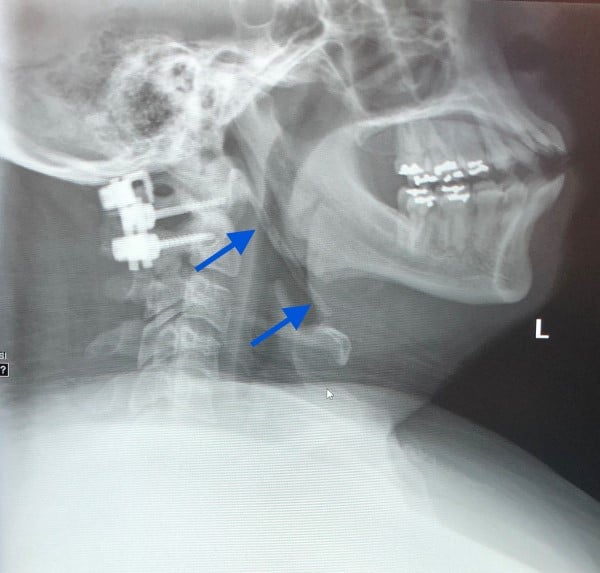
Figure 1
CT or radiographs can both be helpful in diagnosis. CT — especially a 3D-CT scan — is considered superior, given its ability to provide accurate evaluation of the styloid process, its anatomic relationship to surrounding neck structures, and for surgical planning.4 CT will demonstrate a calcified styloid process.3 Radiographs may include panoramic or lateral views. Radiographs will demonstrate a calcified structure extending from the base of the skull toward the hyoid bone.3 On physical exam, the styloid process may be palpated in the tonsillar fossa, as styloid processes that are normal in length are usually not easily palpable. Palpation of styloid process may elicit pain or exacerbation of symptoms.3
Definitive treatment is surgical, requiring styloidectomy to shorten the styloid process via an intraoral or extraoral approach. The intraoral approach has been widely criticized given its increased risk of deep neck space infections and poor visualization of surgical field as it is performed through the mouth. The extraoral approach is preferred, although it may lead to external scarring or facial nerve injuries.6 Surgical styloidectomy has a cure rate of about 80%.6 More conservative, medical management can be guided by symptomatology. Medication includes pain control with NSAIDs, anticonvulsants such as carbamazepine or gabapentin, and SSRIs. Transpharyngeal injection with steroids and anesthetics have also been shown to help with pain. In our case, we also suspected our patient may have a gastroesophageal reflux component, and therefore treated the patient for such.
Case Conclusion
Findings were discussed with the patient, and he was discharged with famotidine and ENT follow up.
References
- Eagle syndrome. Genetic and Rare Diseases Information Center. https://rarediseases.info.nih.gov/diseases/9401/eagle-syndrome. Accessed January 28, 2021.
- Godden DR, Adam S, Woodwards RT. Eagle's syndrome: an unusual cause of a clicking jaw. Br Dent J. 1999 May 22;186(10):489-90. Accessed January 28, 2021.
- Murtagh RD, Caracciolo JT, Fernandez G. CT Findings Associated with Eagle Syndrome. American Journal of Neuroradiology. 2001; 22(7):1401-02. Accessed January 28, 2021.
- Saccomanno S, Greco F, DE Corso E, et al. Eagle's Syndrome, from clinical presentation to diagnosis and surgical treatment: a case report. Acta Otorhinolaryngol Ital. 2018 Apr;38(2):166-169. Accessed January 28, 2021.
- Singh G. Eagle syndrome. Radiology Reference Article. Radiopaedia.org. Radiopaedia Blog RSS. Accessed January 28, 2021.
- Vittorio Rinaldi MD. Eagle Syndrome Questions & Answers. Published January 21, 2021. Accessed January 28, 2021.



