A 54-year-old male with a history of hypertension presents to the ED with palpitations. What is your interpretation of his EKG?
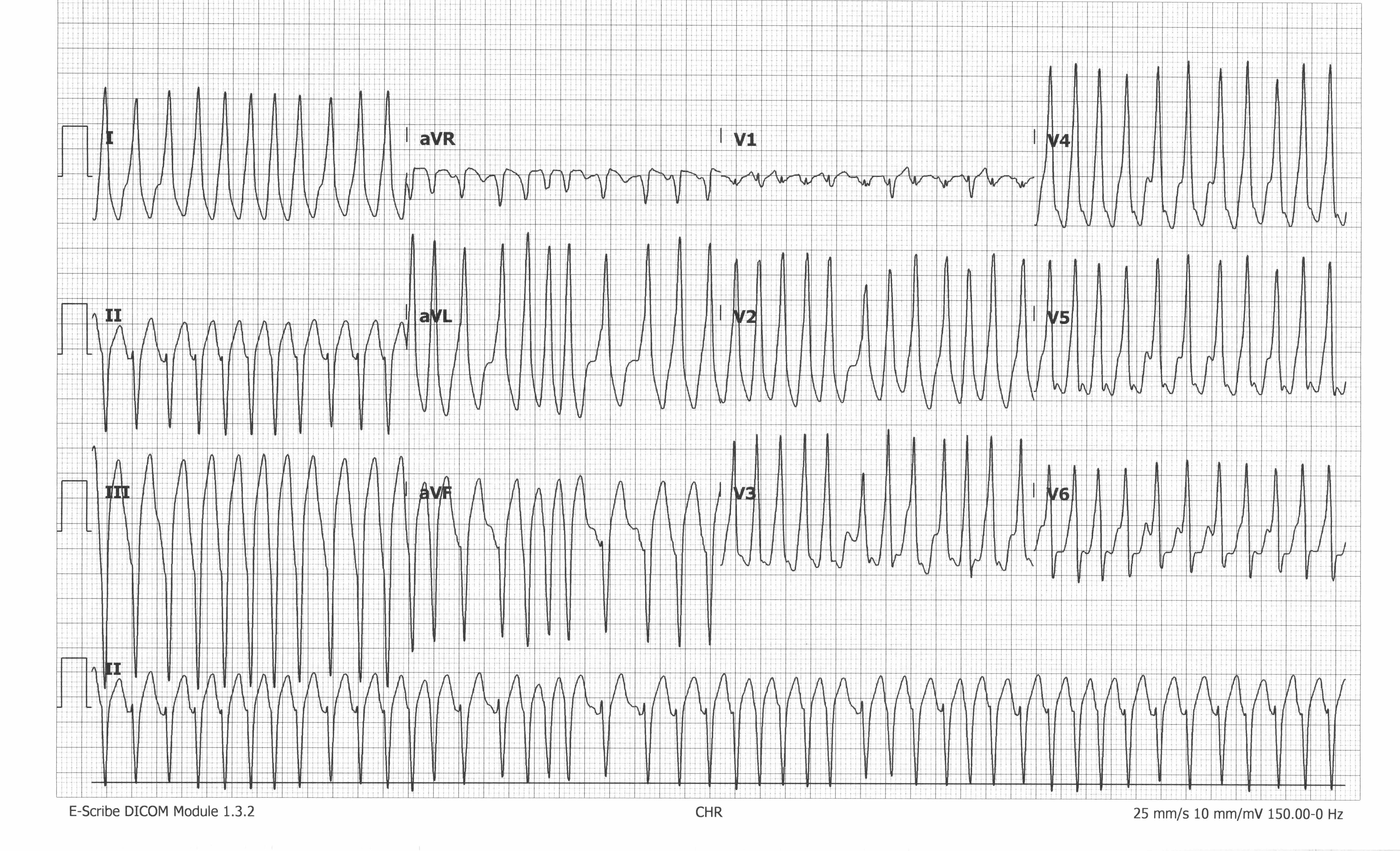
WCT
The EKG shows an irregularly irregular wide-complex tachycardia (WCT) with an average ventricular rate of 270, no obvious P-waves, and left axis deviation. The differential for a very fast irregularly irregular WCT without P-waves is very limited, especially in a patient who is talking and has a measurable blood pressure. The extremely fast ventricular rates, often up to 300 bpm, and presence of delta waves, best seen in aVL, seen on this EKG suggest the presence of an accessory pathway (AP), making AFib with Wolff-Parkinson-White syndrome (WPW) the most likely etiology. Unfortunately, there was no prior EKG for comparison.
The importance of identifying AFib with WPW, and not mistaking it for AFib with aberrant conduction, is due to the treatment. The mainstay of treatment for AFib with RVR (in the absence of an AP) is to slow conduction through the AV node with nodal blocking agents. The role of the AV node in normal cardiac physiology is to slow conduction between the atria and ventricle to maximize ventricular preload via the atrial kick. In AFib, the AV node prevents ventricular rates from exceeding 220-240 bpm in the absence of any extrinsic factors that increase conduction velocity (eg, catecholamine surge or hyperthyroidism). Conduction down the AP is usually faster than the AV node, so in AFib with WPW, the AV node acts as a brake that tempers the faster AP conduction. Nodal blockers don't work very well on the AP, so using them to treat AFib with WPW will allow for increased conduction down the AP that could potentially precipitate ventricular dysrhythmias. The safest treatments for AFib with WPW are procainamide (if the patient is stable) or cardioversion. Procainamide reduces conduction velocity throughout the entire cardiac conduction system, including the AP and ventricle, and inhibits ectopic atrial pacemaker activity. Amiodarone should not be used as it has nodal blocking properties and questionable efficacy on reducing conduction velocity though the AP.
LEARNING POINTS
Irregular Wide Complex Tachycardias
• Rate > 100 bpm, QRS > 120 ms, and variable RR interval
• DDx includes:
- Atrial fibrillation with aberrant conduction (BBB or WPW)
- Atrial flutter with variable block and aberrant conduction
- MAT with aberrant conduction
- Polymorphic ventricular tachycardia
- Ventricular fibrillation
Atrial Fibrillation with WPW
GENERAL FEATURES
• Very fast, irregularly irregular tachycardia
EKG FEATURES
• Ventricular rate typically 180-300 bpm
• Variable QRS morphologies in any single lead
CLINICAL SIGNIFICANCE
• Often misdiagnosed as atrial fibrillation with aberrancy from BBB
• AV nodal blockers should be avoided - can precipitate ventricular fibrillation and cardiovascular collapse
• Procainamide and cardioversion are safe treatment options for AFib with WPW
Case Conclusion
The patient was immediately placed in a room and noted to be diaphoretic and ill-appearing. Initial vital signs showed tachycardia and tachypnea with a slightly elevated blood pressure. The decision was made to treat with cardioversion given his symptoms, clinical appearance, and extreme tachycardia. After successful cardioversion, his symptoms and clinical appearance improved significantly. A repeat ECG showed sinus tachycardia with a short PR interval and initial slurring of QRS (delta wave) consistent with WPW.

Labs were notable for an elevated troponin of 0.13, likely because of demand ischemia, and a low TSH with elevated free T4. During his hospital stay, he was evaluated by endocrinology and diagnosed with Graves' disease, which was thought to be the trigger of his new-onset AFib and likely contributed to the rapid ventricular rates seen on his initial EKG. He later underwent catheter ablation of his AP and was discharged home.



