A 52-year-old male presents to the ED with chest pain. What is your interpretation of his EKG?
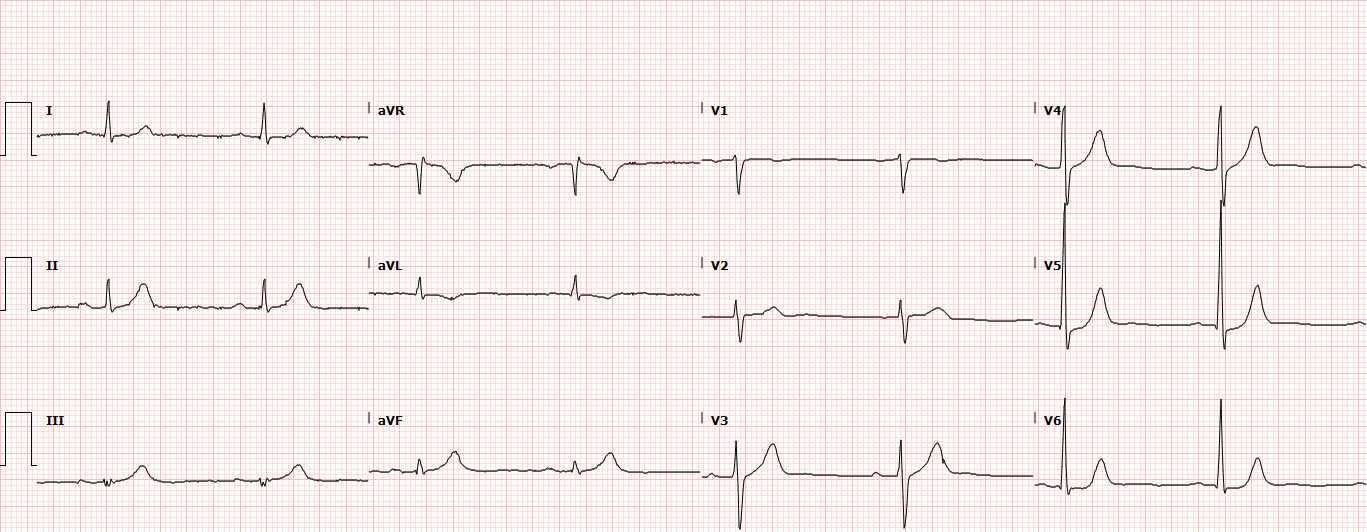
TWI in aVL
Sinus bradycardia with T-wave inversion (TWI) in aVL, hyperacute T waves in the inferior leads, and slight STD in the lateral precordial leads. In a patient presenting with chest pain, these findings are concerning for ischemia and/or impending infarction.
A new isolated TWI in aVL is becoming more commonly recognized as a concerning EKG finding in patients presenting with chest pain. It is critical to be observant for this finding when interpreting an EKG. One study found that 74.9% of physicians missed the finding in their interpretation.1 Reciprocal changes, which include TWI and/or STD, can be the earliest EKG finding for an AMI.
The isolated TWI in aVL is associated with both impending inferior wall MI and mid-LAD lesions. Multiple studies have demonstrated that an isolated TWI in aVL has a high specificity for mid-LAD lesions, and one study one found it to be the only ECG variable significantly predictive of mid-LAD lesion.2 When seen with an inferior MI, reciprocal changes in aVL have a high sensitivity, specificity, and PPV for right ventricular involvement, which is associated with a higher morbidity and mortality.
The “New Tall T-wave in V1” or “Too Tall T-wave in V1” is another EKG finding that can be an early sign of ischemia and/or infarct in patients presenting with chest pain. It can be thought of as an early hyperacute T-wave concerning for impending anterior MI. The T-wave is typically inverted in V1 so a new upright T-wave in V1 (when compared to a prior EKG) or the T-wave amplitude in V1 > V6 are considered abnormal in the absence of LVH, LBBB, or high voltage (eg, young athletes). As with any hyperacute T-waves, serial EKGs should be obtained to see if it evolves.
LEARNING POINTS
Ischemic T-wave Inversions (TWI)
GENERAL FEATURES
• TWI ≥ 0.1 mm in ≥ 2 contiguous leads with prominent R-wave or R/S ratio >1
CLINICAL SIGNIFICANCE
• New TWI (compared to prior) in the setting of a clinically suggestive presentation should prompt concern for ACS
• New upright T-wave ≥ 0.15 mm in V1 is abnormal in the absence of LVH or BBB
- Called “Too Tall T-wave” in ACS presentations and suggests impending anterior ACS
- Upright T-wave in V1 > V6 is concerning for CAD or acute ischemia
• TWI in aVL
- Can be seen with occlusion of mid-LAD
- Potential early indicator of impending inferior MI
- Suggests RV involvement when seen with inferior MI
• When in doubt, obtain serial EKGs
Hyperacute T-waves
GENERAL FEATURES
• No universally accepted definition of hyperacute T-waves
EKG FEATURES
• Tall, prominent T wave with broad base
- Hyperkalemia produces tall, peaked, symmetric, narrow based T-waves
• T wave size is relative to QRS, so small T wave can be hyperacute if paired with a small QRS
• Asymmetric with gradual upstroke (ascending) and abrupt return to baseline (descending)
• J-point elevation
CLINICAL SIGNIFICANCE
• Suggests acute vessel occlusion with ischemia and impending AMI
• In appropriate presentation, EKG indication for reperfusion therapy
• Hyperacute T-waves + ST depression in reciprocal leads ⇒ early AMI
References
1. Hassen GW, Costea A, Carrazco C, et al. Isolated T Wave Inversion in Lead aVL: An ECG Survey and a Case Report. Emerg Med Int. 2015;Article ID 250614. doi http://dx.doi.org/10.1155/2015/250614.
2. Hassen GW, Costea A, Smith T. The Neglected Lead on Electrocardiogram: T Wave Inversion in Lead aVL, Nonspecific Finding or a Sign for Left Anterior Descending Artery Lesion? J Emerg Med. 2014;46(2):165-170.



