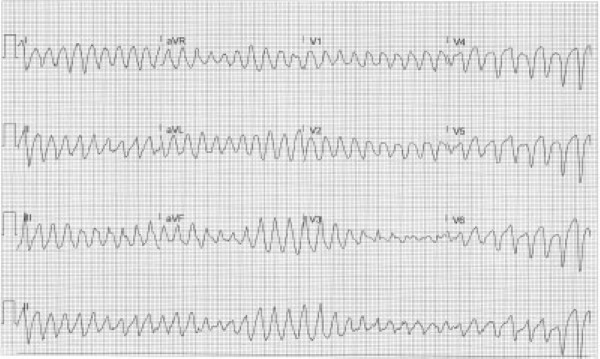
A 68-year-old female with a past medical history of hypertension presents to the emergency department via private vehicle for recurrent intermittent episodes of unresponsiveness that started just prior to arrival. What is your interpretation of her ECG?
ANSWER
This ECG shows an irregular wide complex tachycardia at 230 bpm, no discernible P-waves, and phasic variation (i.e., happens over a number of beats) of the QRS complex axis and amplitude.
The differential diagnosis for an irregular WCT includes:
- Ventricular fibrillation
- Polymorphic ventricular tachycardia (including torsades de pointes)
- MAT with aberrant conduction*
- Atrial flutter with variable block and aberrant conduction*
- Atrial fibrillation with aberrant conduction*
*Causes of aberrant conduction include fixed or rate-related BBB, metabolic abnormalities, sodium channel blocker toxicity, ventricular-paced rhythm, and ventricular pre-excitation (e.g., WPW).
The findings in this ECG are consistent with torsades de pointes (TdP), or “twisting of points,” which describes the characteristic twisting of the peaks of the QRS complexes around the isoelectric baseline. TdP is used to describe polymorphic VT associated with a prolonged QTc interval on the baseline ECG. It is usually paroxysmal and self-terminating, but it can degenerate into ventricular fibrillation. Conversely, non-torsades polymorphic ventricular tachycardia is defined by the absence of a prolonged QTc interval on the baseline ECG. It is often due to ischemia and is constant, frequently leading to hemodynamic compromise.
A prolonged QTc interval is defined ≥ 460 msec for women and ≥ 450 msec for men, with an increased risk for TdP when the QTc interval exceeds 500 msec. The QT interval should be measured in the lead with the longest QT interval, usually lead V2 or V3. Unfortunately, there is no consensus recommendation for which formula should be used to calculate the QTc interval.
The treatment for unstable polymorphic ventricular tachycardia is defibrillation regardless of classification. Intermittent TdP can be treated with magnesium, electrical overdrive pacing, and potassium repletion (if indicated), regardless of whether it is due to an acquired or congenital prolonged QTc interval. TdP due to an acquired prolonged QTc interval can also be treated with chemical overdrive pacing with isoproterenol. This should be avoided in patients with congenital long QT syndrome, as adrenergic stimuli is a common trigger of dysrhythmias. Even though the QTc interval increases with slower ventricular rates, maintenance therapy for these patients commonly includes beta-blockers to minimize adrenergic stimulation. Patients with non-torsades polymorphic ventricular tachycardia should have an ACS workup.
Case Conclusion
While the initial ECG was being obtained, the patient became unresponsive with palpable pulses. While defibrillator pads were being placed, she spontaneously converted to sinus rhythm with a concurrent improvement in her mental status. A repeat ECG showed sinus rhythm with a QTc interval of 515 msec, and she was immediately treated with 4 g IV magnesium sulfate given over 5 minutes. Labs were notable for severe hypokalemia of 1.6 mEq/L, so aggressive replacement was initiated with both oral and IV potassium. The patient was admitted to the cardiology service and had no further episodes of TdP after her potassium level normalized. An echocardiogram showed no abnormalities, and electrophysiology recommended against placement of an implantable cardioverter defibrillator since the dysrhythmia was triggered by a reversible cause.
Polymorphic Ventricular Tachycardia Learning Points
- Irregular WCT with phasic variation (i.e., happens over a number of beats) of the QRS complex axis and amplitude
- Rate is typically 180-250 bpm
- Classified as either torsades or non-torsades
- Torsades de pointes
- Polymorphic VT with a prolonged QTc interval on baseline ECG
- Usually paroxysmal and self-terminating but can degenerate into ventricular fibrillation
- Non-torsades polymorphic VT
- Absence of QTc prolongation on baseline ECG, typically due to ischemia
- Usually sustained and causes hemodynamic instability
- Treatment includes:
- Defibrillation for unstable polymorphic ventricular tachycardia regardless of etiology
- ACS workup for all non-torsades polymorphic ventricular tachycardia
- Magnesium, electrical overdrive pacing, and potassium repletion (if indicated) for intermittent torsades
- Identify and correct underlying cause(s) for torsades (eg, QT prolonging medications, hypokalemia, hypomagnesemia, hypocalcemia, elevated ICP, etc.)



