While approximately 49% of us have male genitalia, nearly all emergency physicians are uncomfortable with penile problems and procedures.
Moreover, it is not easy obtaining volunteers or male colleagues to be the simulated patient during penile procedure day during grand rounds. Because these emergencies occur so infrequently, emergency physicians typically encounter their first penile aspiration or paraphimosis reduction on an actual patient who needs help emergently. But this is why we became emergency physicians – to save life and "limb."
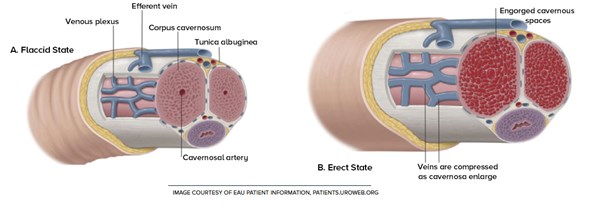
For lack of a better term, a "penile fracture" is defined as a tear in the tunica albuginea of the corpus cavernosum, even though there is no anatomical bone within the penis. This "fracture" typically occurs when an external force is applied to an erect penis, leading to immediate pain and rapid detumescence. Mounting intercourse and aggressive masturbation have been discovered as common causes for a ruptured tunica albuginea.1 The practice of taghaandan is another common cause in Western Iran wherein men forcibly "snap" an erection to force detumescence.2
Eggplant Sign
The eggplant sign is the classic presentation because the penis looks just like the subtropical vegetable due to swelling and extravasation of blood into the superficial tissue of the penis. Ironically, this common distinction has been around long before the invention of emojis. As emergency physicians, there is not much we can do for these patients other than assessing for urethral injury, providing adequate analgesia, and — most important — emergent consultation with urology. If hematuria is present, a cystourethrogram to rule out urethral injury should be completed prior to surgical repair of the penile fracture.
The term priapism is derived from Priapus, the Greek God of fertility, lust, viticulture, and the protector of horticulture (explaining the association with eggplants). Priapism is defined as a persistent erection for at least 4 hours in the absence of sexual stimulation. It can be further classified as either ischemic or non-ischemic, and the distinctive features are further clarified in Table 1.
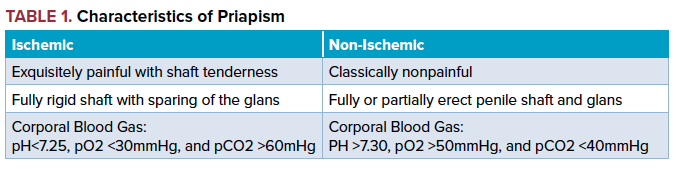
To help distinguish these two types, you can think of ischemic priapism as compartment syndrome of the penis, but please do not attempt a fasciotomy in this case. Stuttering priapism is a subtype of recurrent ischemic priapism that occurs over an extended period of time and is almost exclusively seen in the setting of sickle cell disease.
Non-ischemic priapism is far less common and is most commonly caused by penile or perineal trauma. Non-ischemic priapism is generally self-limiting and resolves within several hours to days. Additional treatments include embolization and surgical ligation, which is beyond the scope of emergency medicine.
Management of Priapism
Ischemic priapism can be managed in the ED with corporal aspiration with or without irrigation and intra-cavernosal injections of phenylephrine. Aspiration/irrigation involves inserting an 18-22 gauge needle connected to tubing and a 3-way stopcock. A butterfly needle tends to work the best as it provides stability of the needle within the corpora cavernosa.
Remove up to 20-40 mL or until bright red arterial blood is aspirated and sterile water can then be injected. For intra-cavernosal injections, 100-500 mcg of phenylephrine is injected directly into the corpora cavernosa.3 In order to obtain the 500 mcg/mL mixture, mix 0.5 mL of phenylephrine (10 mg/mL) in 9.5 mL of normal saline.4
Inject up to 1 mL of the phenylephrine solution every 3-5 minutes for up to one hour until detumescence is achieved.5 Less than 1 mL could be injected for children or patients with coronary artery disease.
If these techniques are unsuccessful, urology should be consulted immediately. Patients with sickle cell disease should also receive disease-specific treatments such as blood transfusions and exchange transfusions if necessary.
Paraphimosis occurs when the penile foreskin in an uncircumcised male becomes entrapped behind the coronal sulcus and cannot be returned to its normal, protracted position. Emergent reduction of the foreskin must be attempted in order to prevent further injury to the glans. Local skin necrosis is the most common outcome, but untimely management could lead to infarction, gangrene, and two words that no man would ever want associated with his penis: auto-amputation.
Analgesia with parenteral opiates, penile dorsal nerve block, and even procedural sedation should be implemented prior to manual reduction of the foreskin. Various methods to reduce swelling of the glans to assist in foreskin protraction include manual compression or wrapping a compressive dressing such as coban around the glans.6 Osmotic agents such as granulated sugar, 50% dextrose, or 20% mannitol could be placed on the glans with application of a compressive dressing to further facilitate swelling reduction.
Overall, penile emergencies are quite uncommon but require rapid treatment. It is imperative that we all routinely familiarize ourselves with these problems and procedures pertinent to the penile emergencies.
References
1. Greenberg MI, Hendrickson RG, Silverberg M. Greenberg's Text-Atlas of Emergency Medicine. 4th ed. Philadelphia, PA: Wolters Kluwer; 2004.
2. Zargooshi J. Penile Fracture in Kermanshah, Iran: Report of 172 Cases. J Urol. 2000;164(2):364-366.
3. Montague D, Jarow J, Broderick G, Dmochowski R, Heaton J, Lue T, Sharlip I. American Urological Association. Management of Priapism. Accessed June 16, 2018.
4. Wieder JA. Pocket Guide to Urology. 4th ed. Caldwell, ID: Griffith Publishing; 2010:456-460.
5. Clavijo-Eisele J. Handbook of On Call Urology. 2nd ed. Urology Solutions Publishing; 2015: 103–107.
6. Little B, White M. Treatment Options for Paraphimosis. Int J Clin Pract. 2005;59(5):591-593.