From intravenous drugs and genetic engineering to highly advanced equipment to mind-blowing surgical techniques, medicine continues to evolve at an exponential pace.
In an almost comedic way, despite this evolution, “good old-fashioned” chest compressions are the only consistent intervention to improve cardiac arrest outcomes.1 Cardiopulmonary resuscitation (CPR), however, is not immune to this omnipresent evolution. We are reviewing a whole new way of performing this life-saving practice: head-up CPR.
Background
The objective of CPR is to take the place of a nonfunctioning heart in delivering blood, and therefore oxygen and other essential products, to the body. Traditionally, the heart is compressed between the sternum, posterior rib cage, and spine supine.2 During the past several years, many theories began to emerge regarding the optimization of this practice. Different experiments were done, mostly in pigs, tracking the amount of blood flow that travels to the brain and other organs depending on certain body positions.3,4 The pigs were sedated and induced into cardiac arrest, after which they underwent CPR in supine, Trendelenburg (head and torso angled inferiorly to rest of body), and reverse Trendelenburg positions. Investigators consistently found that the reverse Trendelenburg position increased perfusion to the brain by 15-20%.5 Interestingly, Trendelenburg resulted in cerebral venous pooling, impeding blood flow and circulation to the brain and reducing venous return subsequent blood flow to other distal organs. Consequently, many of the pigs ended up with cerebral swelling along with a marked decrease in perfusion to the rest of the body.4,6 By angling the body in the opposite direction, venous drainage, and distal perfusion were optimized.
There are three main mechanisms by which head-up CPR is thought to have such profound optimization:
- The primary mechanism of benefit behind head-up CPR is the utilization of gravity in augmenting venous drainage, thereby decreasing ICP and facilitating distal blood flow.6
- The second mechanism of benefit is thought to be the concept of decreasing the concussive force of the blood being thrust into and out of the brain.6 Angling the head upwards decreases these forces.
- A third mechanism involves redistributing blood flow through the lungs in a manner similar to when patients with respiratory distress/failure sit upright (“tripoding”).6 Standing and sitting upright are the ideal positions for breathing and circulation.7 It wasn’t long before these exciting effects made it to the attention of EMS medical directors and fire chiefs.
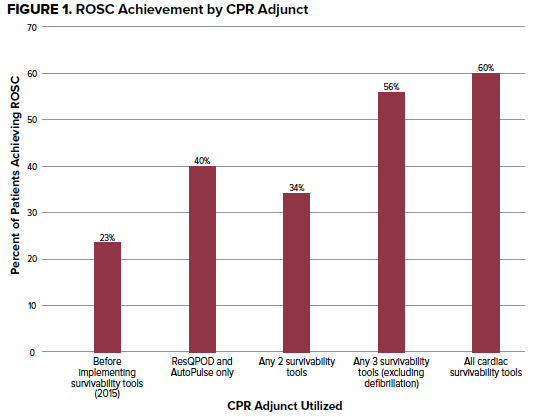
Historically, return of spontaneous circulation (ROSC) rates of out-of-hospital cardiac arrest (OHCA) have ranged between 20-30%.8 In other words, only 20-30% of patients who suffer OHCA ever regain a pulse. According to some studies, many of these patients who regain a pulse only do so for a short period, rarely making it to being discharged from the hospital; survival to hospital discharge (SHD) is around 8-9%.8 Even more unattractive, the neurological outcomes of these few who have survived are almost always dire. In a ground-breaking trial, the Rialto Fire Department (RFD) in California began performing head-up CPR for their cardiac arrest patients. The results have been exhilarating. Previously, Rialto’s ROSC rates were around 23%, meaning that only 23% of cardiac arrest patients ended up regaining a pulse.
Since employing head-up CPR protocol, ROSC rates are averaging 51% for the past three years (2016-2018), regardless of the rhythm the patient was found in, if the arrest was witnessed, or if CPR was applied prior to arrival.9,10 Additionally, SHD has ranged from 12-14%.9,10 Asystole is ubiquitously regarded as the rhythm with the poorest prognosis in cardiac arrest. What is perhaps the most astounding, the RFD rate of ROSC for the initial presenting rhythm of asystole, including unwitnessed arrests, is 26%?10 While the ROSC rates have been extremely encouraging, the next phase of assessment concerns neurological outcomes. Currently, several studies are underway to track the neurological outcomes of OHCA survivors who received head-up CPR. Exploring the neurological benefits of head-up CPR has pragmatic implications as there is often a conflicted sense of accomplishment when achieving ROSC in a patient who has no chance at any sort of neurological recovery.
How to Perform Head-Up CPR
The optimal mechanism for performing head-up CPR has not been rigorously studied yet; however, Rialto has paved the way for a solid starting point. One must first perform CPR flat before elevation, which is thought to prime the cardio-cerebral circuit.6 Once primed, the head is to be elevated 30 degrees. Interestingly, prior pig studies found diminishing returns and harm when elevating the head greater than and below 30°.3 Regarding how to perform the compressions with this new angle, the ideal method is to use an automated CPR device (Lucas, Autopulse, etc.). Performing human-powered chest compressions on an angled patient could potentially compromise the quality of those compressions, especially in the prehospital setting, making these automated CPR devices crucial. Additionally, RFD used an Impedance Threshold Device (ITD).11 This is a small device that attaches in between the ET tube and bag valve. It acts as a one-way valve, allowing oxygen to be delivered during ventilation while restricting ambient air from entering the thoracic cavity during the recoil phase of chest compressions.11 This increases negative intrathoracic pressure creating a vacuum that pulls more blood back to the heart, increasing preload and decreasing intracranial pressure (ICP), allowing for quality cerebral perfusion.12 While theoretically beneficial, when the ITD has been used on its own, studies have been mixed regarding effectiveness and differences in actual outcomes. It appears to have a synergistic and multiplicative effect when used in head-up CPR, however. This synergy seems to be evidenced by abrupt increases in ETCO2 values following ITD placement, head-up CPR already being performed in the setting. However, it is unclear how much of a ETCO2 rise occurs from head-up CPR on its own.10
Capnography and ETCO2 monitoring have long been crucial in guiding CPR quality and prognosis. Generally, ETCO2 > 15 mmHg during CPR is an encouraging value, indicating good compressions and relatively increased chances of ROSC. Below 10 mmHg is usually considered as reasonable evidence to cease CPR.13
The encouraging numbers from RFD may not have been due to head-up CPR alone. RFD developed a set of 7 practices that had to be employed while utilizing head-up CPR:10
- Continuous uninterrupted compressions utilizing an automated CPR device;
- Apneic oxygenation- placement of nasal cannula 15L/min prior to and during ventilations
- Use of an impedance threshold device (ITD)
- Head-up CPR
- Delaying defibrillation for a certain subset of patient presentations- Prolonged downtime patients, fine V-fib, and having ETCO2 reading <20mmhg were not defibrillated. Once ETCO2 20mmhg or greater, or change into shockable rhythm occurred, defibrillation was performed. The theory is that the acidotic heart is less receptive to electrical current.
- Utilization of waveform capnography
- Deprioritizing epinephrine in the order of intervention- Not administering epinephrine until ETCO2 values were ideal and/or until CPR had been underway for a certain period of time. It is believed that by administering epinephrine in less acidic and more perfused environment, it has greater chances of benefit.
Conclusion
The practice of head-up CPR is exciting and encouraging, but much more data is needed before global implementation. RFD continues to utilize head-up CPR and several other fire departments are also implementing it, most notably Palm Beach Fire Department in Florida. Additionally, several studies are currently being conducted in a controlled setting to identify survivability and neurological outcomes14. Perhaps in several years, data will be robust enough to prove or disprove its perceived benefits.
Take-Home Points
- Head-up CPR is showing promising effects in cardiac arrest outcomes.
- 3 main mechanisms of head-up CPR benefit are decreasing cerebral venous pooling, decreasing the concussive force of blood entering the brain during supine CPR, and facilitating blood flow into the lungs (sitting up/standing up is ideal for this), leading to relatively optimal oxygenation.
- Performing head-up CPR requires some special equipment and techniques.
- Several studies are being conducted to draw more definitive conclusions.
References
- 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Accessed July 7.
- Rajab TK, Pozner CN, Conrad C, Cohn LH, Schmitto JD. Technique for chest compressions in adult CPR. World J Emerg Surg. Dec 2011;6:41.
- Rojas-Salvador C, Moore JC, Salverda B, Lick M, Debaty G, Lurie KG. Effect of controlled sequential elevation timing of the head and thorax during cardiopulmonary resuscitation on cerebral perfusion pressures in a porcine model of cardiac arrest. Resuscitation. 04 2020;149:162-169.
- Moore JC, Segal N, Debaty G, Lurie KG. The do's and dont's of head up CPR: Lessons learned from the animal laboratory. Resuscitation. 2018;129:e6-e7.
- Debaty G, Shin SD, Metzger A, et al. Tilting for perfusion: head-up position during cardiopulmonary resuscitation improves brain flow in a porcine model of cardiac arrest. Resuscitation. Feb 2015;87:38-43.
- Moore J. Head-Up CPR May Improve Neurologically Intact Survival Rates. JEMS. 2019. February 14, 2019. Accessed July 7, 2021.
- Katz S, Arish N, Rokach A, Zaltzman Y, Marcus EL. The effect of body position on pulmonary function: a systematic review. BMC Pulm Med. Oct 2018;18(1):159.
- Yan S, Gan Y, Jiang N, et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020;24(1):61.
- Grayson S. Rialto Fire Department Changes the Paradigm of Cardiac Arrest. JEMS. 2019. Accessed July 7, 2021.
- Powell J, Grayson S, Dearden K. Seven Tools Result in Dramatic Improvements in Cardiac Arrest Outcomes in Rialto, Calif. JEMS. 2017.
- ResQPOD ITD. Accessed July 7, 2021,
- Metzger AK, Herman M, McKnite S, Tang W, Yannopoulos D. Improved cerebral perfusion pressures and 24-hr neurological survival in a porcine model of cardiac arrest with active compression-decompression cardiopulmonary resuscitation and augmentation of negative intrathoracic pressure. Crit Care Med. 2012;40(6):1851-6.
- Rabjohns J. End-Tidal CO2 in Cardiopulmonary Resuscitation. 2019. February 6, 2019. Accessed July 7, 2021.



