ED Facility Fee Price Transparency Shows Opportunities for Policy Change
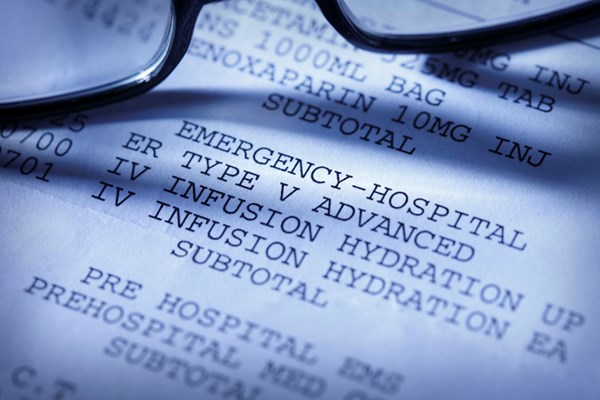
Advocacy efforts for equitable health care often focus on access to care. However, an important, yet understudied population are those who self-pay – choosing not to, or being unable to, bill insurance for their health care. This exposes these patients to vulnerability associated with emergent and acute care, as they do not benefit from price negotiations, and instead are often billed discounted cash prices – the maximum charges for a service.
Because these patients are not included in payer databases, a major source of health services research, little is known about their demographics and the degree to which their financial responsibilities are affected by regional and hospital characteristics.
A recent study addresses some of these unknowns by leveraging recent publicly available data from the Turquoise Health academic license hospital price transparency data set – published in accordance with recent legislation making posting prices mandatory. They chose to investigate cash prices associated with ED facility fees. Every ED patient encounters these fees, which are set at the discretion of the hospital, thus providing insight into how these fees may vary with bed size, health system affiliation, and ownership status among other characteristics. The data include prices from 1,621 hospitals and reveal several interesting findings:
- Median cash price for ED facility fees ranged from $160.78 (CPT code 99281, low-level ED visits) to $1,097.43 (CPT code 99285, highest-level ED visits).
- Higher cash prices were associated with for-profit hospitals, hospitals with more than 250 beds, and health system-affiliated hospitals for ED visit levels 3–5.
- Facility fees were significantly lower for ED visit levels 2–5 at hospitals in counties with higher poverty rates.
Though the authors did attempt to adjust for this, these data may be incomplete as fewer than 37% of hospitals have cash prices posted for all care levels, despite mandates in effect since January 2021. This lack of disclosure could signify an area of need for policy advocacy efforts. While facility fees only make up a portion of patients' total ED-related costs, the variability in these prices are adjustable and are responsive to local markets – indicating a potential point of policy. The unexpected nature of emergent care negates the possibility of searching for the best prices, and may lead to avoid seeking care, and adverse impacts on patients' health.
ABSTRACT
Henderson MA, Mouslim MC. Hospital and regional characteristics associated with emergency department facility fee cash pricing. Health Aff (Millwood). 2022;41(7):1029-1035.
Background: Self-pay patients are an understudied yet important and financially vulnerable population of emergency department (ED) users. As ED facility fees may be a key cost driver in patient ED bills, we leveraged newly available hospital pricing data to describe ED facility fees for self-pay patients (cash prices) and how they vary according to hospital and regional characteristics in a sample of 1,621 hospitals across the United States.
Findings: The median cash price for ED facility fees ranged from $160.78 for a level 1 visit to $1,097.43 for a level 5 visit. Hospital for-profit status and a bed count of 251 or more beds were associated with higher cash prices for ED facility fees across all visit levels. Meanwhile, location in a county with a poverty rate of 16% or more was correlated with lower facility fee cash prices for ED visit levels 2 and up.
We hope these findings can inform targeted policy efforts to better ensure affordable ED care for vulnerable patients Medicare Hospital Readmissions Reduction Program (HRRP) financially penalizes hospitals with high readmission rates. In fiscal year 2019 the program was changed to account for the association between social risk and high readmission rates. The new approach stratifies hospitals into 5 groups by the hospitals' proportion of patients dually enrolled in Medicare and Medicaid, and it evaluates performance within each stratum instead of within the national cohort. Its impact on hospitals caring for vulnerable populations has not been studied.
EMRA + PolicyRx Health Policy Journal Club: A collaboration between Policy Prescriptions and EMRA
 As emergency physicians, we care for all members of society, and as such have a unique vantage point on the state of health care. What we find frustrating in our EDs - such as inadequate social services, the dearth of primary care physicians, and the lack of mental health services - are universal problems. As EM residents and fellows, we learn the management of myocardial infarctions and traumas, and how to intubate, but we are not taught how health policy affects all aspects of our experience in the ED. Furthermore, given our unique position in the health care system, we have an incredible opportunity to advocate for our patients, for society, and for physicians. Yet, with so many competing interests vying for our conference education time, advocacy is often not included in the curricula. This is the gap this initiative aims to fill. Each month, you will see a review of a new health policy article and how it is applicable to emergency physicians.
As emergency physicians, we care for all members of society, and as such have a unique vantage point on the state of health care. What we find frustrating in our EDs - such as inadequate social services, the dearth of primary care physicians, and the lack of mental health services - are universal problems. As EM residents and fellows, we learn the management of myocardial infarctions and traumas, and how to intubate, but we are not taught how health policy affects all aspects of our experience in the ED. Furthermore, given our unique position in the health care system, we have an incredible opportunity to advocate for our patients, for society, and for physicians. Yet, with so many competing interests vying for our conference education time, advocacy is often not included in the curricula. This is the gap this initiative aims to fill. Each month, you will see a review of a new health policy article and how it is applicable to emergency physicians.