The bill a patient receives is more complicated than just the physician bill. It has multiple parts, and - depending on other services used during an ED visit - they may contain a few different charges. It's important to understand how a bill is generated, what procedures can be billed, and how to optimize your documentation.
Emergency medicine residents are used to learning and incorporating different practice styles of the various physicians we work with: one day we might be admitting every case of the “man flu” and the next we are discharging every patient we see. Education on documentation and billing is frequently no different, and we frequently must learn on the fly with tips from attendings during shift. Most programs lack a curriculum on billing, even though many post-residency jobs have at least partial compensation tied to physician productivity. The goal of this article is to increase basic knowledge of what goes into a patient’s hospital bill, how billing for an emergency physician is determined, how to optimize documentation for billing, what procedures can be billed, and what may qualify for critical care time.
What's in a Bill?
The bill a patient receives is more complicated than just the physician bill. It has multiple parts, and - depending on other services used during an ED visit - they may contain a few different charges. This bill consists of:
- The facility fee: charges for hospital usage, supplies, medications given, radiology studies performed, and nursing staff
- Physician’s professional fees: can include multiple physician groups (for example, if radiology provided a CT interpretation or another service was consulted in the ED)
Documentation and Coding 101
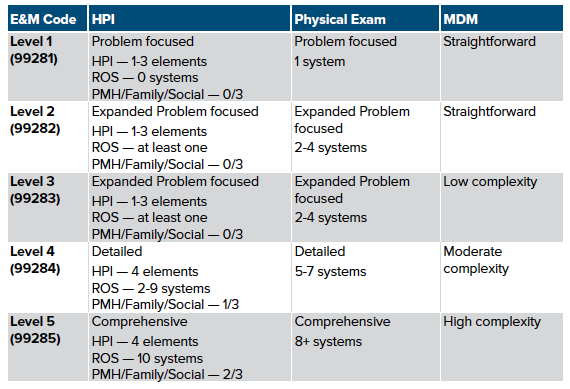
We've all been completing charts detailing patient encounters since the first day of residency. So how is billing linked to your documentation? For the emergency department most patient encounters end up being linked to an Evaluation and Management code (E/M code), and each code has a certain reimbursement level. E/M codes range from 1 (extremely simple encounter) to 5 (complex encounter). To determine the billing level, each section of the chart is assigned a level of complexity. Sections include:
- History of Presenting Illness
- Chief complaint
- History
- ROS
- Past medical/surgical history, family history, social history
- Physical Exam
- MDM
Once each is assigned a level, the chart will be billed at the lowest level out of all sections. So for example, if the chart is a level 5 complexity for all sections, but your ROS is only a level 3, the chart will end up being billed as a level 3. With this example it’s easy to see how a few small things can lead to a LOT of lost reimbursement!
What Exactly Dictates the E/M Level of a Chart?
Each chart is assigned a code level based on the complexity of each section. The way CMS determines complexity level for each section generally pertains to the number of components you document in each section. Below is a chart detailing documentation requirements for each of the levels. HPI and PE sections are show, and MDM will be discussed in a later section, as it is slightly more complicated.
MDM Complexity Levels
Medical decision making is the last aspect of the chart (almost done, take a deep breath!), which contributes to the overall billing level. Interpreting the complexity of the MDM is a little more nebulous compared to the concrete requirements for the HPI and PE sections. The process is performed when a coder reviews the MDM section and attempts to determine how complex the case was based off of:
- Risk of presenting complaint with respect to morbidity/mortality
- Number of diagnostic/management options considered
- Complexity of data analyzed and ultimate disposition
In general the elements are combined and can be estimated using the table below:
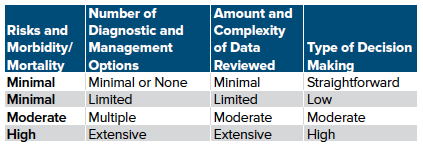
Each aspect can be split and analyzed separately, as shown.
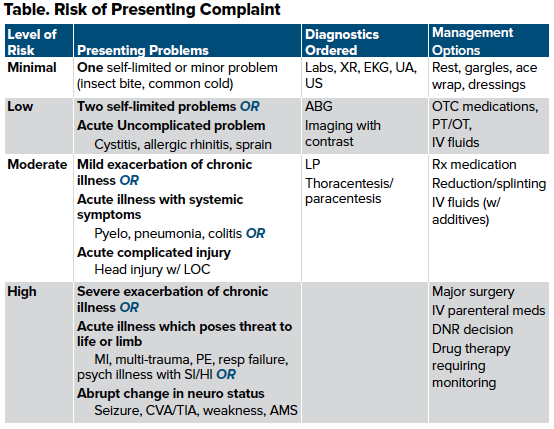
Number of diagnostic/management options considered
This section generally refers to the potential diagnoses being considered and the assumed level of investment needed to investigate those diagnoses. An unofficial scoring tool (the Marshfield Clinic Scoring Tool) was developed to guide the complexity of a proposed problem. To simplify, essentially any new problems will either be moderate or high complexity. If there is any workup planned it will be considered high complexity. Any established issues such as asthma or COPD without intervention will generally be low or moderate. Of note, an exacerbation of a chronic issue would be considered new.
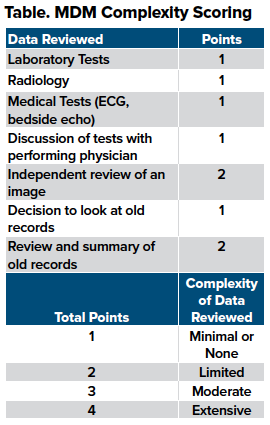
Complexity of data analyzed and ultimate disposition
Any description of your thought process and information you used to guide your decision will be weighed in a scoring system to evaluate the complexity of data review. It is important to put your own brief interpretation for a test for it to be included in the complexity score. Be sure to note things such as XR, CT, and ECG even if you have an official read from a consultant. The table shows the type of data to include, along with how a coder will score it.
MDM can get confusing and somewhat complicated in terms of billing and coding. It also is likely the most important aspect of your chart in terms of billing level.
To make sure your chart is billed appropriately, include all of the work and thought you put into a patient. Remember to:
- Summarize important differentials you were considering
- Briefly explain why you gave certain medications
- Summarize laboratory, ECG, and radiology results
- If you looked through previous charts, give a brief explanation
- Make sure to mention risk to your patient, even if they end up being diagnosed with a more benign condition (eg, that pregnant vaginal bleed could have been an ectopic, but ultimately was diagnosed with threatened abortion)
Take-Home Points
- Emergency training is rightly geared toward education, growth, and being the best physician you can be. As of now the paucity of education in billing means every resident must be vigilant in learning how to document correctly.
- Knowledge of appropriate billing will affect graduating residents who have some influence of the RVU on their compensation.
- Make sure to document correctly and with adequate detail to ensure you are reimbursed for all of the work you do.
- For the history and physical sections of your chart, make sure you document (and perform, of course!) the appropriate number of systems to support the assumed level of billing.
- For the MDM, include your emergency differentials, summary of information processed, and any risk the patient could have had from their condition.
- As a side note, macros are your friend; just make sure they are accurate for your patient. This cannot be overstated. Insurance companies are pushing back on macros!
- Make sure you detail information for your specific patient, especially in the MDM. Good luck and bill well!



