Immune thrombocytopenia (ITP) can often be first diagnosed and recognized in an ED setting, both as a primary and incidental finding. Let's review a typical presentation and the unique pathology and specific treatment for this diagnosis.
CASE REPORT
A 67-year-old woman presents to the emergency department for evaluation of a lower extremity rash. The patient was in her usual state of good health prior to presentation before the gradual onset of decreased energy and arthralgias accompanied by nasal congestion, rhinorrhea, poor appetite and concerns she had a recent viral upper respiratory infection. The evening prior to presentation, the patient noted multiple petechiae around her ankles bilaterally which spread to involve the both legs up to her knees by morning. She has had no fever, chills, neck pain, photophobia, neck stiffness, epistaxis, cough, shortness of breath, chest pain, abdominal pain, vomiting, signs of gastrointestinal bleeding, hematuria, or lower extremity swelling. She did note frequently tasting blood in her mouth after brushing her teeth over the past day. The patient has a past medical history significant for rheumatoid arthritis, migraines, and acid reflux. The patient’s medications included acetaminophen and omeprazole, with no new or different medications.
On exam, the patient was a pleasant elderly woman in no apparent distress. Physical exam was unremarkable except for ulnar deviation of the proximal and distal interphalangeal joints consistent with her prior diagnosis of rheumatoid arthritis and lower extremity exam revealing dark purple petechiae measuring 1-2 mm each scattered throughout her bilateral lower extremities (Figure 1a and 1b).


Laboratory investigation revealed thrombocytopenia below the detectable level of 3,000/L. There were no other cell count abnormalities, and electrolytes, renal function tests, and INR were all within normal ranges.
The patient was diagnosed with suspected primary ITP without signs of active bleeding and received a dose of 50 mg of oral prednisone in the ED and was admitted to the hospital due to a critically low platelet count. Her hospital course consisted of daily doses of 50mg oral prednisone and a single dose of intravenous rituximab. The patient’s hospital course was otherwise unremarkable and the patient’s platelet count had returned to 94,000/L on the fifth day. The patient was discharged to home on oral prednisone after six days of hospitalization with close follow-up at an outpatient hematology clinic.
DISCUSSION
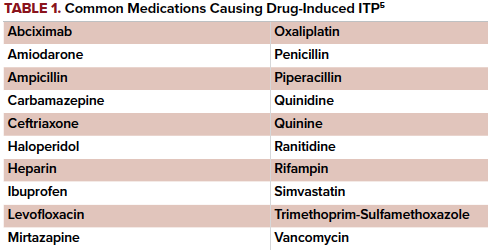
In the setting of isolated thrombocytopenia unexplained by another condition, a diagnosis of Immune Thrombocytopenia (ITP) can be made. Immune Thrombocytopenia (formerly known as Idiopathic Thrombocytopenia Purpura) is an autoantibody-mediated destruction of platelets and associated decreased release of platelets from megakaryocytes. A platelet count of less than 100,000/L is required for a diagnosis of the 3 types of ITP: primary, secondary, and drug induced.1 Primary ITP is not caused by any other underlying condition or drug reaction. Secondary ITP is in the setting of systemic disease- common etiologies include HIV, Hepatitis C, systemic lupus erythematosus or leukemia and often improves with treatment of the underlying disease.1 ITP can often also be seen in conjunction with other autoimmune disorders, including rheumatoid arthritis,2 as was the case for this patient. Drug-induced ITP is a medication-induced antibody reaction causing platelet destruction (see Table 1 for common offending agents).
Overall severity of illness is correlated to platelet levels, though severe ITP is clinically defined as cases with significant bleeding requiring intervention.3
Typical presentations will include petechiae or purpura that develop over days, usually associated with platelet counts less than 20,000/L.3 Other presentations include persistent superficial bleeding or recurrent bruising, epistaxis, gingival bleeding, hematuria, or menorrhagia.4 The risk for spontaneous or traumatic intracranial hemorrhage or internal bleeding is highest in patients with platelets levels less than 10,000/L.4 One pooled analysis of ITP patients with persistent platelet levels less 30,000/L showed a predicted 5-year mortality rate from fatal hemorrhage of 2.2% for patients younger than 40 and 47.8% for patients older than 60.6 Patients with platelet counts above 50,000/L are typically asymptomatic and thrombocytopenia is usually an incidental finding.4 Studies have shown that most cases are diagnosed in the fifth to sixth decade of life with a higher incidence in women; however, one-third to one-fifth of cases of ITP are diagnosed incidentally without symptoms, therefore true prevalence is difficult ascertain.7
Treatment of ITP has 2 major focuses: bleeding control and increasing platelet levels. Bleeding control follows direct local pressure or packing pending on the site as would be done for non-thrombocytopenic patients. One recent case series has shown the potential for improved homeostasis with the use of intravenous tranexamic acid (TXA) in ITP patients with active bleeding.8 Platelet transfusion should be considered in any significant bleed, especially in the setting of platelet counts less than 30,000/L.9 Transfusion should not be initiated in patients without active bleeding, regardless of platelet count. 9 However, platelet transfusions in asymptomatic patients with ITP are not associated with the higher morbidity and mortality seen in other platelet-consumptive processed such at thrombotic thrombocytopenic purpura (TTP) or heparin-induced thrombocytopenia (HIT).10 One unit of platelets should increase total count by 30,000-50,000/L. 9 Ideally, platelet transfusion should be given with intravenous immunoglobulin (IVIG) over several hours in discussion with a hematology consultant.4 In patients presenting with minor bleeds with platelet counts less than 20,000/L, initial treatment should include IV methylprednisolone (40 mg for adults) for several days or oral prednisone (1 mg/kg) to be continued for several weeks with taper.4 Hospitalization is at discretion of provider but required for patients with significant mucocutaneous or internal bleeding and those who have a platelet count less than 20,000/L with a history of prior significant bleed.4
Relapses of thrombocytopenia are not uncommon and can occur following recent infection (as was seen in our case) and also treated with corticosteroids or IVIG. Complete response to treatment is achieved when platelet counts are between 30,000 -100,000/L with at least double the baseline count.3 Cases with refractory bleeding or severe thrombocytopenia despite glucocorticoids and IVIG may be considered for treatment with Factor VIIa11 or biologics such as Rituximab4 as this patient received.
TAKE-HOME POINTS
- Consider ITP in patients with petechiae (often lower extremity) or recurrent bruising, epistaxis, gingival bleeding, hematuria, or menorrhagia.
- A platelet count of less than 100,000/L is required for a diagnosis and consider new drugs or disease processes as causes before diagnosing primary ITP.
- Initial treatment should include IV methylprednisolone (40mg in adults) or oral prednisone (1mg/kg). Consider platelet transfusion in those with active bleeding and admission for those with bleeding or critically low levels (<20,000/L).
- Predicted 5-year mortality rates ranged from 2.2% for patients younger than 40 years to 47.8% for those older than 60 years.
REFERENCES
- Cooper N, Bussel J. The pathogenesis of immune thrombocytopenic purpura. Br J Haematol. 2006;133(4):364-374.
- Ichikawa N, Harigai M, Nakajima A, et al. Immune thrombocytopenic purpura associate with rheumatoid arthritis – a report of five cases and review of the literature. Mod Rheumatol. 2001; 11(3):246-250.
- Rodeghiero F, Stasi R, Gernsheimer T, et al. Standardization of terminology, definitions and outcome criteria in immune thrombocytopenic purpura of adults and children: report from an international working group. Blood. 2008; 113(11):2386-2393.
- Cines D. How I treat idiopathic thrombocytopenic purpura (ITP). 2005;106(7): 2244-2251.
- Arnold DM, Kukaswadia S, Nazi I, et al. A systematic evaluation of laboratory testing for drug-induced immune thrombocytopenia. J Thromb Haemost. 2013;11(1):169-176.
- Cohen YC, Djulbegovic B, Shamai-Lubovitz O, Mozes B. The Bleeding Risk and Natural History of Idiopathic Thrombocytopenic Purpura in Patients with Persistent Low Platelet Counts. Arch Intern Med. 2000;160(11):1630-1638.
- Portielje JE, Westendorp RG, Kluin-Nelemans HC, Brand A. Morbidity and mortality in adults with idiopathic purpura. Blood. 2001; 97(9): 2549-2554.
- Mayer B, Salama A. Successful treatment of bleeding with tranexamic acid in a series of 12 patients with immune thrombocytopenia. Vox Sang. 2017;112(8):767-772.
- Estcourt LJ, Birchal J, Allard S, et al. Guidelines for the use of platelet transfusions. Br J Haematol. 2017;176(3):365-394.
- Goel R, Ness PM, Takemoto CM, Krishnamurti L, King KE, Tobian AAR. Platelet transfusions in platelet consumptive disorders are associated with arterial thrombosis and in-hospital mortality. Blood. 2015;125(9):1470-1476.
- Čulić, S. Recombinant factor VIIa for refractive haemorrhage in autoimmune idiopathic thrombocytopenic purpura. Br J Haematol. 2003;120(5):909-910.