Kawasaki Disease and Multisystem Inflammatory Syndrome (MIS-C) can be challenging to distinguish. Ongoing studies are helping emergency physicians better understand how to recognize and manage MIS-C in pediatric patients.
Case 1: A 10-month old female with no past medical history presents to the Emergency Department (ED) with fever and rash. Her father notes fever for the past 5 days. Yesterday evening she developed a rash. Today she has decreased fluid and solid intake. Her father brought her to see the pediatrician who recommended an evaluation in the ED. Her vitals reveal a temperature of 38.0°C, a heart rate of 120 bpm, a blood pressure of 90/60 mmHg, a respiratory rate of 24, and a SPO2 of 97% on room air. On exam the patient has conjunctival injection, red cracked lips, swollen hands/feet, and an erythematous papular rash to her back.
Case 2: A 9-year-old male presents to the ED with fever and abdominal pain. His mother reports the patient has had fever for 2 days and increasing abdominal pain. Today, the patient had three episodes of non-bloody, non-bilious emesis. The mother reports that he tested positive for SARS-CoV-2 three weeks ago. His vitals reveal a temperature of 38.7°C, a heart rate of 149 bpm, a blood pressure of 92/50 mmHg, a respiratory rate of 34, and a SPO2 of 91% on room air. On exam the patient is very uncomfortable-appearing. The abdomen is noted to be soft but with guarding and tenderness to palpation in all quadrants. There was no rash present.
Epidemiology and Pathophysiology
Kawasaki Disease (KD) is a systemic vasculitis of unknown etiology. Approximately 80% of cases are in children less than 5 years old with peak incidence at 18-24 months of age. KD is rare in children less than 6 months of age.1 Incidence is highest among Asians and Pacific Islanders.2 Medium-sized arteries are most affected, particularly the coronary arteries. Blood vessel damage appears to result from inflammatory cell infiltration into vascular tissue of unknown stimulus. This leads to disruption in the structural integrity of the arterial wall due to the loss of elastin and collagen fibers. 3
Multisystem inflammatory syndrome in children (MIS-C) is a hyperinflammatory syndrome associated with SARS-CoV-2; 70% of MIS-C cases occur in patients greater than 5 years old with a peak incidence between 5 and 9 years of age. Hispanic/Latino and non-Hispanic Black patients account for approximately 70% of cases.4 Pathophysiology of MIS-C is not well understood and likely results from an abnormal immune response to a SARS-CoV-2 infection in the preceding weeks.5 The diagnosis may be challenging as some patients may have been asymptomatic during their primary SARS-CoV-2 infection. 6 MIS-C shares clinical similarities with KD. However, based on literature review, MIS-C appears to have a different immunophenotype than KD.7
Signs and Symptoms
KD has a well described classic set of criteria used in establishing the diagnosis. In order to meet diagnostic criteria, patients must have a fever for 5 days or greater. Additionally, patients must meet at least four of the signs and symptoms listed in Table 1. These signs and symptoms usually do not present in a particular order. Clinicians should be aware and vigilant for the possibility of incomplete KD (iKD) which may be present despite patients not meeting at least 4 of the necessary signs and symptoms. The diagnosis of iKD requires laboratory data and often includes echocardiogram and expert consultation in aiding in the diagnosis. The most common cardiac manifestation is tachycardia out of proportion to the degree of fever.8 Blood pressures are mostly within normal limits. Rarely, patients may present in or develop Kawasaki Disease Shock Syndrome in which hypotension is present.9
Table 1. Diagnostic Criteria for KD
The diagnosis of Kawasaki Disease requires the presence of fever lasting at least 5 days with no other explanation, combined with at least 4 of the 5 following criteria:
- Bilateral bulbar conjunctival injection
- Oral mucous membrane changes (injected or fissured lips, injected pharynx, strawberry tongue)
- Peripheral extremity changes (erythema of palms or soles, edema of hands or feet, periungual desquamation)
- Polymorphous rash
- Cervical lymphadenopathy at least 1 lymph node > 1.5 cm in diameter
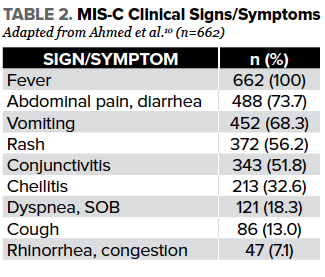
The presentation of MIS-C is less straightforward as it may mimic other emergent conditions. Fever is universal in MIS-C patients as described in a recent systematic review of a cohort of 662 patients; however, there is no defined fever length as is seen in KD at current.10 In the same systematic review, it was described that gastrointestinal symptoms are very common and seen in up to 73% of cases. Contrary to acute COVID-19, the majority of patients with MIS-C lack significant upper respiratory symptoms.11 Other clinical signs and symptoms according to the recent systematic review can be found in Table 2. What is particularly notable in MIS-C is the high number of patients that present in shock or are initially stable only to rapidly decompensate in the ED or the inpatient setting.10
Initial Workup & Evaluation
Diagnostic evaluation of patients with KD is clinical. Laboratory workup is indicated when iKD is suspected but the patient does not meet the initial diagnostic criteria. This workup includes complete blood count with differential, erythrocyte sedimentation rate (ESR), c-reactive protein (CRP), liver function tests, albumin and urinalysis with microscopy. iKD is associated with elevated ESR/CRP, leukocytosis, anemia, thrombocytosis, sterile pyuria, elevated aspartate transaminase (AST), and hypoalbuminemia.
Diagnosis of MIS-C is more difficult, and ED providers should have a high index of suspicion in the ongoing COVID-19 era. Initial workup of MIS-C should be similar to that of patients with sepsis. MIS-C and sepsis are often indistinguishable in the ED setting. This includes blood cultures, assessment for end-organ dysfunction, and labs to assess for a hyperinflammatory state. A suggested work-up can be seen in Table 3.
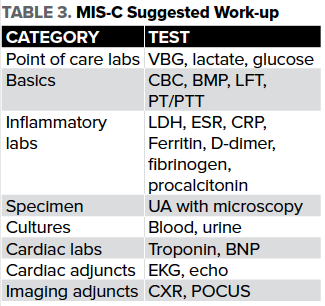
Additionally, patients should have a baseline electrocardiogram and echocardiogram. Bedside point-of-care ultrasound (POCUS) can be helpful in providing quick estimates of both cardiac function and responsiveness to fluid resuscitation. Of note, some MIS-C patients may be fluid non-responsive and serial POCUS exams may help the ED provider anticipate the need for vasopressor support. Imaging studies including chest x-ray can be helpful in the patient presenting in respiratory distress to rule out other sources of infection. Given that a large number of patients present with severe gastrointestinal symptoms, a formal ultrasound and/or CT scan of the abdomen/pelvis may be necessary to rule out other common diagnoses such as appendicitis.
Treatment and Disposition
Treatment for patients with KD includes intravenous immune globulin (IVIG) and aspirin (ASA). A commonly dosed regimen for IVIG is 2 g/kg.12,13 For ASA, initial and maintenance dosing regimens vary across institutions. 14 It is important to note that treatment should align with established hospital protocols. Most KD patients are appropriate for admission to the pediatric floor. If there is evidence of shock, such as seen in Kawasaki Disease Shock Syndrome, the pediatric intensive care unit (PICU) may be more appropriate. There are institutional variations in the consultants involved in the care of KD patients. Usually at a minimum, cardiology is needed for echocardiography to evaluate the coronary arteries. Some institutions may involve infectious disease and rheumatology in patient management.
For MIS-C, treatment in the ED should include judicious fluid administration while serially reevaluating for responsiveness or evidence of worsened cardiac function. Additionally, given sepsis cannot be excluded, empiric broad-spectrum antibiotics are recommended in ill-appearing patients. Many patients may require some oxygen supplementation and vasopressor support.10 It is important to note that management of MIS-C requires a multidisciplinary team.15 When MIS-C is suspected in the ED, PICU and cardiology consults are generally indicated. Approximately 60-70% of MIS-C patients require intensive care admissions at some point during their hospital stay so involving the PICU early is useful.10,16 Generally, the infectious disease service is consulted when MIS-C is suspected. Depending on the institution, hematology, rheumatology, and allergy/immunology may be a part of the care team. For patients with severe cardiac dysfunction, activation of an ECMO team may be necessary. Patient disposition should be considered carefully. Medical centers without the multidisciplinary services listed above should consider early transfer of the patient to a regional pediatric center with access to all these services. The decision to admit to the pediatric floor versus the PICU should be made using similar indications to other disease processes. However, consultation with the PICU is reasonable for all patients being admitted with suspected MIS-C, given the high rates of rapid decompensation.10 With early resuscitation and close monitoring, patients with MIS-C tend to do well. According to recent systematic reviews, mortality is estimated at 1.7-1.8%.10,16 Future research and following patients prospectively will be necessary in determining any long-term sequelae of MIS-C.
Case 1 Conclusion
You are confident in the diagnosis of KD. Infectious disease is consulted, and they recommend administration of IVIG. You begin an IVIG infusion and admit to the general pediatric floor service. High-dose aspirin was started on admission. On the wards, an echocardiogram is performed demonstrating normal coronary arteries and an EF of 66%. No other significant findings were noted. The patient was discharged on hospital day 3 on daily aspirin with plans to follow up with the primary care pediatrician and cardiology.
Case 2 Conclusion
Sepsis protocol was initiated. The patient was placed on 4 L oxygen via nasal cannula and saturations improved to 97%. IV access, labs, urine, and blood cultures were obtained. A fluid bolus was given. Ceftriaxone and vancomycin were given to cover for bacterial sepsis. Metronidazole was added as a perforated appendix was considered in the initial differential. A second bolus was given for ongoing tachycardia. A cardiac POCUS showed an IVC without collapsibility. A central line was placed to deliver a vasopressor. An ECG demonstrated sinus tachycardia. CBC noted leukocytosis; VBG was normal; however, lactate was elevated. CRP, Ferritin, D-dimer, fibrinogen were all abnormal. High-sensitivity troponin was normal with a mildly elevated BNP. Blood chemistries were significant for normal creatinine and GFR. Small elevations in AST and ALT were present. PT and PTT were normal. CT of the abdomen and pelvis revealed hepatomegaly and hepatic inflammation, plus multifocal bilateral renal lesions concerning for possible pyelonephritis. The patient was admitted to the PICU for IVIG, steroids, prophylactic anticoagulation, and continued vasopressor support. Formal echo showed an EF of 45% without abnormalities of coronary arteries. ID, hematology, rheumatology, allergy/immunology were consulted. After 6 days in PICU followed by floor, the patient was discharged with appropriate follow-up.
References
- Wu MH, Lin MT, Chen HC, Kao FY, Huang SK. Postnatal Risk of Acquiring Kawasaki Disease: A Nationwide Birth Cohort Database Study. J Pediatr. 2017;180:80-86.e2.
- Nakamura Y. Kawasaki disease: epidemiology and the lessons from it. Int J Rheum Dis. 2018;21(1):16-19.
- Jennette JC, Falk RJ. The role of pathology in the diagnosis of systemic vasculitis. Clin Exp Rheumatol. 2007;25(1 Suppl 44):S52-S56.
- Centers for Disease Control & Prevention. Multisystem Inflammatory Syndrome (MIS-C). Accessed 29 January 2020.
- Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395(10237):1607-1608.
- Feldstein LR, Rose EB, Horwitz SM, et al. Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. N Engl J Med. 2020;383(4):334-346.
- Lee PY, Day-Lewis M, Henderson LA, et al. Distinct clinical and immunological features of SARS-CoV-2-induced multisystem inflammatory syndrome in children. J Clin Invest 2020; 130:5942.
- McCrindle BW, Rowley AH, Newburger JW, et al. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals From the American Heart Association. Circulation 2017; 135:e927.
- Gatterre P, Oualha M, Dupic L, et al. Kawasaki disease: an unexpected etiology of shock and multiple organ dysfunction syndrome. Intensive Care Med. 2012;38(5):872-878.
- Ahmed M, Advani S, Moreira A, et al. Multisystem inflammatory syndrome in children: A systematic review. EClinicalMedicine. 2020;26:100527.
- Hoang A, Chorath K, Moreira A, et al.COVID-19 in 7780 pediatric patients: A systematic review. EClinicalMedicine. 2020;24:100433.
- Newburger JW, Takahashi M, Beiser AS, et al. A single intravenous infusion of gamma globulin as compared with four infusions in the treatment of acute Kawasaki syndrome. N Engl J Med. 1991;324(23):1633-1639.
- Terai M, Shulman ST. Prevalence of coronary artery abnormalities in Kawasaki disease is highly dependent on gamma globulin dose but independent of salicylate dose. J Pediatr. 1997;131(6):888-893.
- McCrindle BW, Rowley AH, Newburger JW, et al. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals From the American Heart Association [published correction appears in Circulation. 2019 Jul 30;140(5):e181-e184]. Circulation. 2017;135(17):e927-e999.
- Dove ML, Jaggi P, Kelleman M, et al. Multisystem Inflammatory Syndrome in Children: Survey of Protocols for Early Hospital Evaluation and Management. J Pediatr. 2021;229:33-40.
- Godfred-Cato S, Bryant B, Leung J, et al. COVID-19-Associated Multisystem Inflammatory Syndrome in Children - United States, March-July 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1074-1080.