As SARS-CoV-2 spreads globally, physicians are turning to different imaging modalities to assist in the diagnosis of COVID-19 and risk stratification of patients. Along with clinical suspicion, chest radiography (CXR), computed tomography (CT), and point-of-care ultrasound (POCUS) are being used in varying degrees to assist in diagnosis while awaiting confirmatory lab results.
CXR is the predominant imaging modality being utilized, but has been found to exhibit a poor sensitivity of 59%, while CT has been shown to have a sensitivity of as high as 86% - 97%.1,2 However, CT in suspected COVID patients has disadvantages such as increased cost, risk of iatrogenic transmission, and in the case of severely ill patients, the risks associated with transporting these patients. In Italy and China, ultrasound has been used as an effective tool in the triage, diagnosis, and the assessment of lung improvement in affected patients. The attendant advantages of bedside US in COVID-19 are multiple; a timely diagnostic modality providing immediate information, real-time capability to monitor improvements and guide treatment, low relative cost, and the absence of radiation.3 In this brief review, we go over some basics of lung ultrasound and the current literature on the ultrasound findings associated with COVID-19.
Basics of Lung Ultrasound
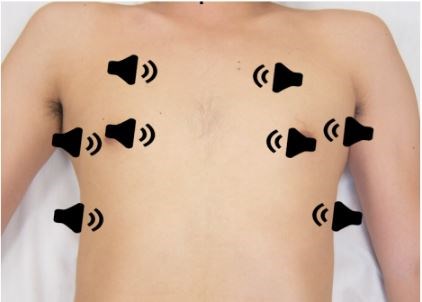
Before covering the sonographic findings of COVID-19, let’s review the basics of lung ultrasound. To start, curvilinear or linear probes are preferred options. The suggested best practice is to use a linear probe for superficial structures and curvilinear probe for deeper structures (diaphragm or pleural effusions) given the latter’s improved depth of penetration.1,2,3 Lung ultrasound has been described as an eight zone technique, but other variations occur (see Figure 1 below). Views in each quadrant may include both longitudinal and transverse views.4
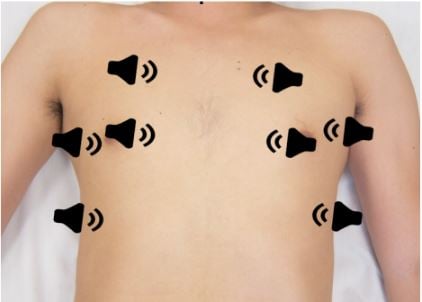
Figure 1. Transducer positioning for the 8 lung zones. Aspler, A. Heslop, C., Stone, M. 2015. PV Card: Focused Lung Ultrasound. ALiEM.5
|
Tips to Optimize Lung POCUS6 |
|
1. For general lung evaluation, use a low frequency curvilinear transducer with a "lung" preset. If a curvilinear transducer is not available, use a phased array low frequency transducer 2. To visualize the pleural line in detail, you may need to use a linear probe. Recommend depth settings of 7-10 cm with a lung preset 3. Scan with the transducer orientation marker in the cephalad direction. To view an area more in-depth, you can turn the probe transversely 4. Check all the chest zones and do not forget to scan the lower posterior lung fields bilaterally |
Begin in the sagittal plane with the probe indicator oriented cephalad. An optimal view will show the hyperechoic pleural line between two ribs that display prominent shadowing.3 Non-pathologic, aerated lung will demonstrate lung sliding, as parietal and visceral pleura glide past one another. Use of M-mode at this interface will demonstrate the "seashore sign" in normal lung as compared to the "barcode sign" in the setting of pneumothorax.7
Aerated lung will also reveal multiple hyperechoic lines at regular intervals deep to the pleural line, known as “A-lines” (see Figure 2 below). These are reverberation artifacts caused by acoustic reflections between the probe and the pleural line. They are a normal finding in healthy individuals.3
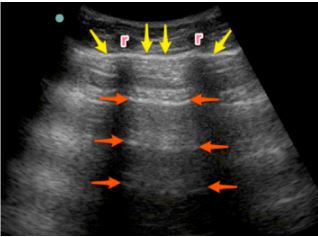
Figure 2. The A-lines are demonstrated by the orange arrows that are visualized as hyperechoic, horizontal artifacts at the regular intervals deep to the pleural line (yellow arrows). There are two ribs (r) in the image.5
“B-lines” are another artifact that are described as long, well-defined, laser-like, hyperechoic lines that originate from the pleural line and move with lung sliding.3 B-lines start at the pleural line and travel to a depth of at least 8 -10 cm. In addition, B-lines move back and forth with respiration as the pleural line moves. They will initially appear as thin single, vertical lines (see Figure 3 below), however, with more interstitial fluid, the lines can coalesce and become more wedge-shaped.3 Greater than three B-lines in each lung field is pathologic and suggests Alveolar-Interstitial Syndrome (AIS) caused by various disease processes including pulmonary edema, lung contusion, interstitial fibrosis, and acute respiratory distress syndrome (ARDS).7,8
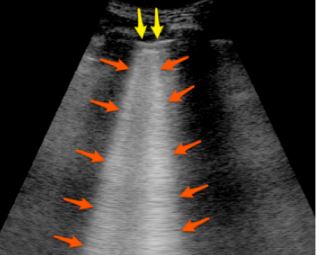
Figure 3. The B-lines (orange arrows) are visualized as hyperechoic vertical artifacts arising from the pleural line (yellow arrows) and extending off the screen without fading, erasing the A-line pattern.5
B-lines and pleural irregularities are often the first sonographic finding seen in COVID-19 pneumonia and can develop into outright consolidations. These findings are discussed in the following section.
Lung Ultrasound in COVID-19
Lung POCUS has been increasingly utilized for COVID-19 patients. The most common symptoms found with COVID-19 include fever, dry cough, and shortness of breath. Most patients who present to the ED only have mild symptoms (80%), whereas 14% present with severe disease, and 5% become critically ill as per the latest WHO reports.9 Of the hospitalized COVID-19 patients, almost all present with distinctive clinical characteristics that progress in a similar way on CT and ultrasound. During COVID-19 disease progression, changes to the lung parenchyma begin in the peripheral regions of the lung and progress centrally. The below chart is adapted from Smith et. al, and differentiates typical sonographic characteristics and clinical characteristics based off the severity of COVID-19 related lung injury.4
|
Disease Severity |
Clinical Characteristics |
Ultrasound Findings |
|
Mild to Moderate |
• Respiratory rate >30 • spO2 ≤ 93% on room air • Typically, will require supplemental O2 • Lung tissue begins to lose aeration |
• Development of B-lines which begin to increase in number and distribution • Pleural line begins to become more irregular • Small <1 cm consolidation |
|
Severe |
• spO2 ≤ 93% on supplemental O2 • Start to show signs of respiratory distress • Increase need of supplemental O2 or respiratory support • Lung tissue is becoming progressively de-aerated |
• B-lines that continue to increase in number and distributions as well as more coalescent and confluent • Begin to affect the upper and anterior areas of the lungs • Small consolidations increase in number & size |
|
Critical |
• Requiring invasive mechanical ventilation • Need high fraction of inspired O2 • Dependent areas of lung tissue have progressively de-aerated |
• Extensive coalescent B-lines • Postero-basilar lungs develop. Significant bilateral alveolar interstitial syndrome progressing to consolidations with or without air bronchograms • Pleural effusions are small or rare unless the patient’s fluid balance is high, they have concomitant CHF, or they have superimposed bacterial infections |
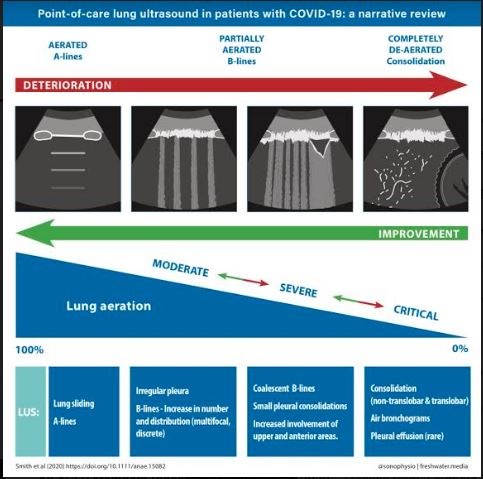
Figure 4. Sonographic characteristics of moderate, severe, and critical pleural and parenchymal changes in patients with COVID-19.4
Multiple studies out of China corroborate these common lung ultrasound characteristics seen in COVID-19. Peng et al compared CT and ultrasound features of patients with COVID-19 pneumonia and demonstrated CT findings corroborating the disease progression seen on ultrasound. The most common findings seen on CT include a thickened pleura, ground glass opacities, pulmonary infiltrating shadow, subpleural and translobar consolidations, and frequent bilateral involvement. A patient can have a negative or atypical lung CT scan in the early stages of the disease.12
|
Most Common Lung Findings in COVID-1911,12 |
|
1. Thickening of the pleural line with pleural line irregularity 2. Subpleural consolidations that can interrupt pleural line 3. B-lines in variety of patterns (focal, multifocal, and confluent) 4. Possible air bronchograms seen in the consolidation 5. Possible predominance in dependent locations (posteriorly and at bases) 6. Re-appearance of A lines during recovery phase 7. Pleural effusions are uncommon |
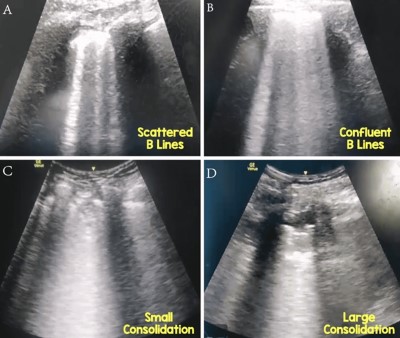
Figure 5. Multiple images from a patient who is COVID-19 positive.12
Limitations of Lung POCUS in COVID-19
There are some limitations of lung ultrasound that must be considered. Lung ultrasound is limited in its ability to detect lesions deep in the lung parenchyma, while abnormalities extending to the pleural surface are more readily visualized. Definitive detection of deeper lesions may require CT scan.12 Infection control is another important consideration, as ultrasound machines, like any other surface, can theoretically become fomites. Institutions should implement best practices to clean the machine to be able to use it between multiple patients. These measures should include limiting the number of probes in the room, using probe covers during aerosolizing procedures, and paying particular attention to both cleaning and disinfection. Some hospitals are designating ultrasound machines for COVID-19 patients only. For more details on mitigating nosocomial spread and proper cleaning with regards to ultrasound in COVID-19, see the ACEP Guideline on COVID-19: Ultrasound Machine and Transducer Cleaning.
Conclusion
Lung POCUS is becoming more popular in COVID-19 patients to aid in diagnosis and characterization of severity of disease. As the incidence and prevalence of COVID-19 pneumonia fluctuates within the community, there is potential for ultrasound to play a role in prognosticating and risk-stratifying patients in the ED, especially those who toe the divide between requiring inpatient monitoring and outpatient follow-up. Further prospective studies are required to appraise this application.
References
- Guan W, Ni Z, Lian W, Ou C., et al. Clinical Characteristics of Coronavirus Disease 2019 in China. The New England Journal of Medicine. 2020;382(18):1708-1720. doi:10.1056/NEJMoa2002032
- Ai T, Yang Z, Hou H, et al. Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases [published online ahead of print, 2020 Feb 26]. Radiology. 2020;200642. doi:10.1148/radiol.2020200642
- Dawson, M. and Mallin, M. Lung. Introduction to Bedside ultrasound: Volume 1. Emergency Ultrasound Solutions; 2013: 66-84
- Smith, M.J., Hayward, S.A., Innes, S.M. and Miller, A.S.C. (2020), Point‐of‐care lung ultrasound in patients with COVID ‐19 – a narrative review. Anaesthesia. doi:1111/anae.15082
- Aspler, A. Heslop, C., Stone, M. PV Card: Focused Lung Ultrasound. ALiEM. https://www.aliem.com/pv-card-focused-lung-ultrasound/. Published August 3, 2017.
- Rao, V. COVID-19 and the Role of Point of Care Ultrasound. Point-of-Care Ultrasound Certification Academy. https://www.pocus.org/covid-19-and-the-role-of-pocus. Published April 24, 2020.
- Lichtenstein, D. BLUE-Protocol and FALLS-Protocol. Chest. 2015;147(6):1659-1670. doi:10.1378/chest.14-1313
- Dietrich CF, Mathis G, Blaivas M, et al. Lung B-line artefacts and their use. J Thorac Dis. 2016;8(6):1356‐ doi:10.21037/jtd.2016.04.55
- World Health Organisation. Coronavirus disease 2019 (COVID19) Situation Report – 41. 1 March 2020. https://www.who.int/d 8
- Poggiali E, Dacrema A, Bastoni D, et al. Can Lung US Help Critical Care Clinicians in the Early Diagnosis of Novel Coronavirus (COVID-19) Pneumonia? Radiology. 2020;295(3). doi:10.1148/radiol.2020200847.
- Huang Y, Wang S, Liu Y, et al. A Preliminary Study on the Ultrasonic Manifestations of Peripulmonary Lesions of Non-Critical Novel Coronavirus Pneumonia (COVID-19). SSRN Electronic Journal. February 2020. doi:10.2139/ssrn.3544750.
- Peng Q-Y, Wang X-T, Zhang L-N. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Medicine. 2020;46(5):849-850. doi:10.1007/s00134-020-05996-6.