Malaria is a rare diagnosis in the U.S. As such, providers outside of infectious disease specialists or those with experience in travel medicine or global health may not be familiar with the disease.
Case
A 19-year-old male presents with a friend to your metropolitan emergency department with 4 days of intermittent fevers, chills, body aches, vomiting, and now altered mental status. The patient's friend thinks he has been otherwise healthy but tells you that the patient recently returned from a trip to Uganda building wells. The patient appears ill on initial assessment, with a heart rate of 123 bpm, blood pressure of 95/68 mmHg, an oxygen saturation of 95% on room air and febrile to 104.5℉. On exam he repeatedly asks where he is but is unable to answer questions. Other than tachycardia and slight tachypnea he has a normal cardiopulmonary exam. His abdomen is non-tender but you do note a palpable liver edge lower than expected. He is moving all extremities but non-compliant with an in-depth neurological exam. The rest of his physical exam was unremarkable and his friend did not know of any other past medical history. Laboratory workup revealed a significant leukocytosis, mild anemia, and elevated creatinine as well as AST and ALT.
Background
Malaria is a rare diagnosis in the U.S. As such, providers outside of infectious disease specialists or those with experience in travel medicine or global health may not be familiar with the disease. Malaria is caused by several Plasmodium species including P. falciparum, P. vivax, P. ovale, P. malariae, and P. knowlesi. The parasite itself is carried and transmitted through bites from the Anopheles mosquitos, often occurring at night. While malaria was previously found across the globe, including in the United States and Europe, currently it is only endemic to tropical and equatorial countries in Africa, Asia and South America.
In the U.S., malaria is rare with the CDC reporting roughly 2,000 new cases in 2016. However, the number of cases in the US has slowly risen since the 1970s, in large part due to increased international travel. Many of those who are traveling are visiting friends and family living abroad; this group was the majority of new cases in 2016. Often those visiting friends and family in malaria-endemic countries may have grown up there and even had malaria as children.
Of the 2,000 cases in the U.S. in 2016, 14% were severe and 7 of the cases (<0.5%) died. While the overall number of cases remains low in the U.S., the WHO estimates that in 2018 there were 405,000 deaths worldwide from malaria with children making up two-thirds of those cases. Malaria remains a major public health threat across the globe.
Clinical Features
There are no symptoms specific to malaria. Uncomplicated malaria most commonly presents with fevers in addition to generalized malaise, myalgias, arthralgias, and mild respiratory and gastrointestinal symptoms. Temporal patterns to the fevers associated with malaria have been classically taught as indicative of the specific Plasmodium species, however, this has been largely disproven. Indeed the fever pattern can be variable in all cases of malaria regardless of species. Symptoms in returned travelers typically develop within a month of returning from an endemic area. However, symptoms can be delayed for up to 6 months in patients infected with P. vivax. The physical exam may show hepatosplenomegaly, jaundice, icterus, or even petechiae. However, there are no specific exam findings to suggest malaria.
A subset of patients will develop severe malaria, encompassing hemodynamic changes and multisystem organ failure. This is a true medical emergency and a presentation emergency physicians should be familiar with. Severe malaria is more common in P. falciparum infections and in patients from non-endemic countries. Severe malaria requires prompt diagnosis and empiric treatment to stave off significant morbidity or mortality. A particularly worrisome variant of severe malaria is cerebral malaria. The pathophysiology is a complex interaction between the infected erythrocytes, cerebral inflammation, and a breakdown of the blood-brain-barrier. The hallmark of cerebral malaria is altered mental status and can progress to seizures. Behavioral changes, neurologic deficits, and epilepsy are potential long-term sequelae of the disease. Other possible presentations of severe malaria include ARDS, renal failure, severe anemia, coagulopathies, and shock (often termed algid malaria). Hypoglycemia has been noted as a potential complication, particularly in pediatric patients.
Diagnosis
There are multiple ways to diagnose malaria. Rapid Diagnostic Tests (RDTs) are antigen-based assays commonly found across the globe. They are particularly sensitive for P. falciparum but may miss other species. Furthermore, they cannot differentiate most Plasmodium species other than P. falciparum & P. vivax. RDTs are a qualitative test and do not reflect the level of parasitemia which may be prognostic in some patients.
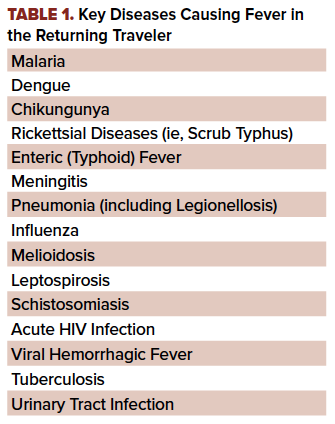
The gold standard for diagnosis remains direct visualization via thick and thin blood smears. In the hands of an experienced microscopist, smears may be more sensitive than RDTs. Direct visualization is also needed for specific species identification outside of P. falciparum and P. vivax, as well as determining parasite burden. Malaria can be definitively ruled out with three negative thick and thin smears obtained over 24-72 hours. Of course, malaria is just one of several infectious diseases that cause fever in the returning traveler. Providers should consider other causative etiologies (Table 1) pending on clinical presentation and travel history.
Treatment & Disposition
Once the diagnosis is made, either through RDT or smear, treatment should be started in the emergency department in conjunction with an infectious disease specialist. If one is not available the CDC’s Operation Center and local public health departments may be able to provide guidance. The choice of treatment is largely based on the causative species, where the infection was obtained, and whether or not the patient was on prophylaxis. If the patient was on prophylaxis an alternative agent should be chosen.
For all but P. vivax, artemether-lumefantrine or atovaquone-proguanil should be sufficient. If unavailable, quinine with doxycycline or clindamycin can be used. Chloroquine is an antiquated treatment given widespread resistance. If P. vivax or P. ovale are suspected based on geographical risk factors or confirmed with testing then primaquine must be added to treat hepatic hypnozoites (a latent form of the parasite). Primaquine should be avoided in patients with G6PD deficiency, which has been found to be protective against certain forms of malaria. In patients with severe malaria, parenteral artesunate is preferred but must be obtained from the CDC given its status as an orphan drug. Generally, in the US it is common that malaria patients are admitted for 24 hours observation even if only mild symptoms are present on the initial presentation. This facilitates speciation, parasite burden determination, and adequate treatment plans. Those with severe malaria should be considered for admission to the ICU.
Prophylaxis guidelines, should you need to prescribe it, can be found through the CDC’s Yellowbook (link in the references). The most common prophylactic medications include atovaquone/proguanil, doxycycline, mefloquine, primaquine, and tafenoquine. Key considerations in choosing a chemoprophylactic agent include the country being visited, length of stay, and side effects of the chosen medication. Atovaquone/proguanil and doxycycline tend to be the most well-tolerated, with the exception of the increased sun sensitivity from doxycycline. Mefloquine, while also effective, is known to have potentially severe neuropsychiatric side effects however has better compliance as dosing is weekly rather than daily. Primaquine and tafenoquine are very effective against P. vivax (the species with most resistance) but require prior G6PD testing. Like most insect-transmitted diseases, prevention is key. Beyond prophylactic medications, travelers in high-prevalence areas should consider using insect repellent, treating clothing with permethrin, and particularly with the night-biting Anopheles mosquito, sleeping under a bed net.
Case Conclusion
While in the ED the patient underwent IV fluid resuscitation and showed interval improvement in hemodynamics and mental status. An RDT came back positive for P. falciparum. With the improvement of his mental status, the patient was able to provide further details including that he had skipped several days of his malaria chemoprophylaxis. He was started on artemether-lumefantrine after consultation with the infectious disease service and admitted to the ICU. He had a short, uncomplicated ICU course followed by a brief ward stay prior to being discharged home.
Take-Home Points
- Malaria is a potentially life-threatening disease to consider in the febrile returning traveler.
- Signs and symptoms can present up to a month after returning from an endemic country.
- Thorough travel, exposure, and prior chemoprophylaxis history are key to diagnosis and treatment.
- Prompt diagnosis and treatment are potentially lifesaving and should be done in consultation with an Infectious Disease expert or CDC.
Disclaimer
The views expressed in this case report are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government. I am a military service member. This work was prepared as part of my official duties. Title 17 U.S.C. 105 provides that "Copyright protection under this title is not available for any work of the United States Government." Title 17 U.S.C. 101 defines a United States Government work as a work prepared by a military service member or employee of the United States Government as part of that person's official duties.
References
- Mace KE, et al. Malaria Surveillance — United States, 2016. MMWR. Surveillance Summaries, vol. 68, no. 5, 2019, pp. 1–35.
- Fink D, et al. Fever in the Returning Traveller. BMJ. 2018.
- Thwaites GE, Day NPJ. Approach to Fever in the Returning Traveler. N Engl J Med. 2017;376(6):548–560.
- Huang F, Scaggs A, Schlaudecker E. Fever in the Returning Traveler. Infectious Disease Clinics of North America. 2018;32(1):163–188.
- Molyneaux M. Malaria. Tintinalli's Emergency Medicine Guide , edited by Judith Tintinalli et al., 8th ed., McGraw-Hill Education, 2016, pp. 1070–1076.
- Louicharoen C, Patin E, Paul R, et al. Positively selected G6PD-Mahidol mutation reduces Plasmodium vivax density in Southeast Asians. Science. 2009;326(5959):1546-1549.
- D’Andrea SM, De Wulf A. Global Travelers. Tintinalli's Emergency Medicine: A Comprehensive Study Guide, 9e Eds. Judith E. Tintinalli, et al. McGraw-Hill, 2020.
- Centers for Disease Control. https://wwwnc.cdc.gov/travel/page/yellowbook-home-2014.



