Fournier's gangrene is a rare, life-threatening condition with a high mortality rate. Save a life by knowing the signs and the most effective interventions.
A 54-year-old female with a significant medical history of hypertension, tobacco dependence, and Type II diabetes presents to the ED complaining of right groin pain. She notes fullness to her right labia and upper thigh for the past week, along with subjective fever and chills. She reports a fullness-type sensation moving in her groin and progressively getting worse. The review of systems is negative for any trauma, abdominal pain, vomiting, vaginal bleeding, vaginal discharge, or any history of similar symptoms.
On physical examination, the patient is afebrile, heart rate of 98 bpm, blood pressure of 140/97, respiratory rate of 21 breaths/min, pulse oximetry on room air of 100%, and a weight of 433 lbs. She is in no acute distress, sitting up in bed, and talkative. The cardiovascular and respiratory findings are unremarkable. The patient is found to have moderate induration of the anterior right labia, extending up to the right inferior portion of the mons pubis. No palpable fluctuance, no evidence of skin necrosis, no crepitance, no drainage, and no bullae are noted. Pain appears out of proportion to the physical exam. No other acute findings are found on physical exam.
Given the history and physical exam, code sepsis was activated, antibiotics were initiated (vancomycin, clindamycin, and piperacillin/tazobactam), and general surgery was immediately contacted for suspected necrotizing fasciitis. A complete blood count revealed a neutrophilic leukocytosis of 23.6 and a mild anemia of 12.7 g/dL. On chemistry, she was found to have a hyponatremia of 130 mmol/L, glucose of 188 mg/dL, a blood urea nitrogen level of 41 mg/dL, and a creatinine of value of 2.30 mg/dL (up from a baseline of 0.70 mg/dL). In addition, she was found to have a lactic acid of 1.5, c-reactive protein of 408 mg/L, and lactate dehydrogenase of 370 U/L. Urinalysis demonstrated cloudy urine, specific gravity of 1.021, 1+ blood, 2+ leukocyte esterase, 11-24 WBC/hpf, and 1+ bacteria. The remainder of the laboratory investigation was unremarkable.
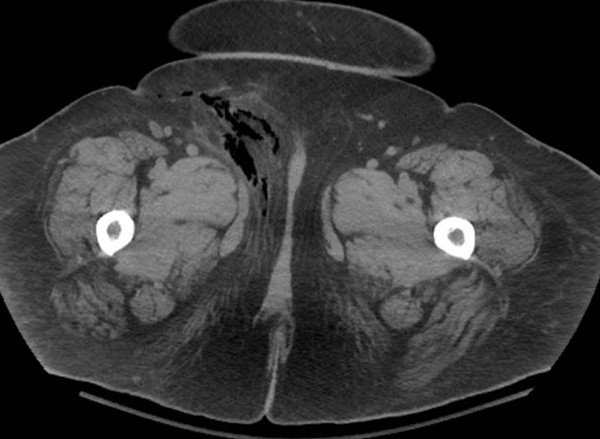
CT abdomen/pelvis without contrast (see Figures 1-3) revealed extensive inflammatory stranding involving the anterior/lateral right pelvic soft tissues with soft tissue gas identified tracking from the lateral right pelvis soft tissues at the level of the iliac crest medially and inferiorly down to the level of the right groin.
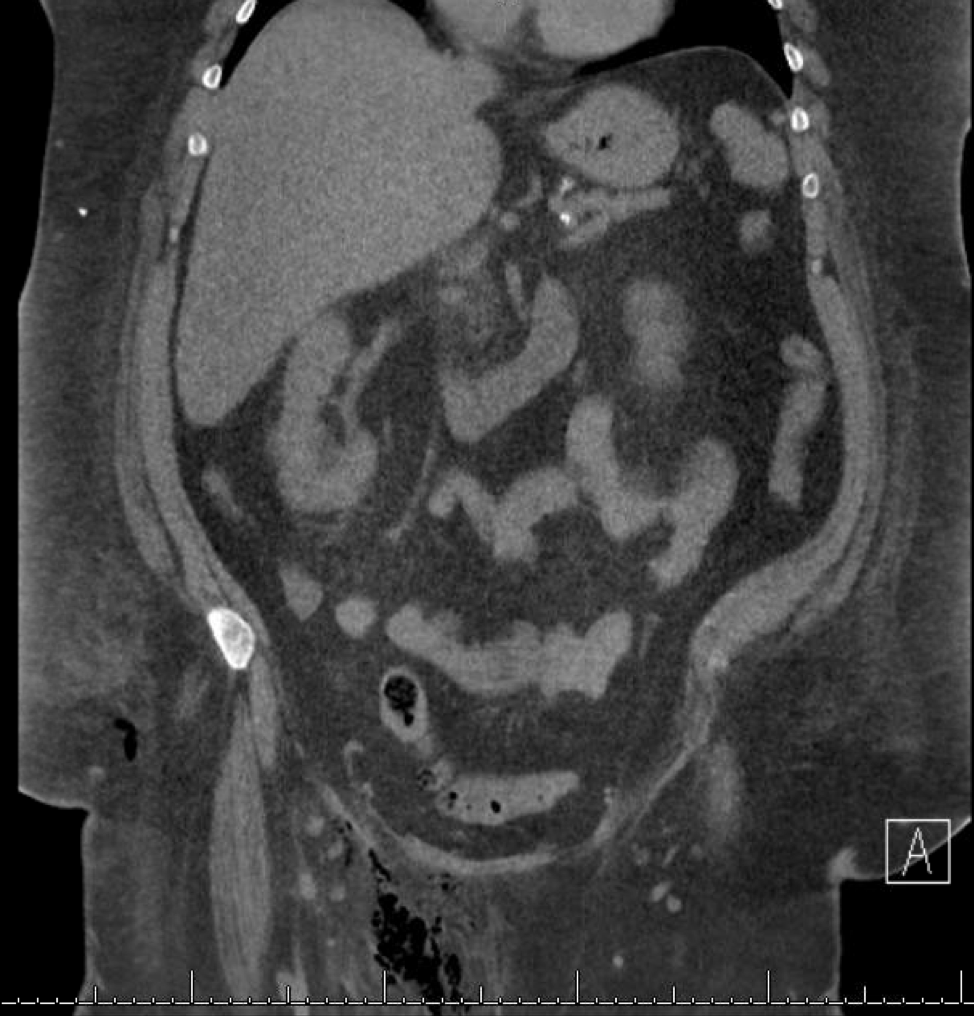

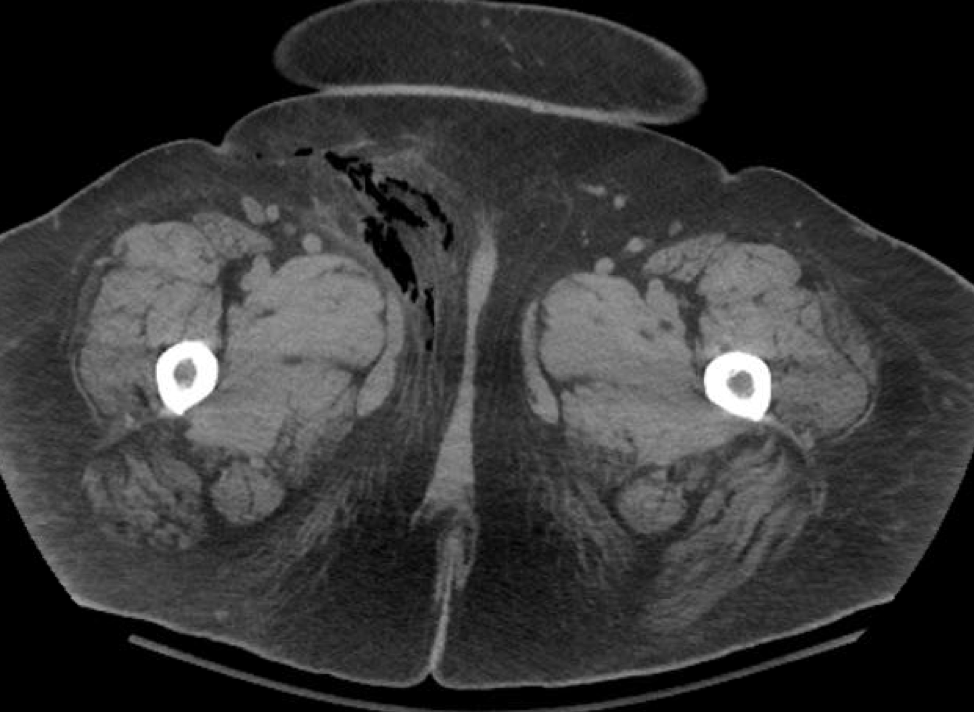
The inflammatory stranding reached the anterior rectus fascia without intraperitoneal extension. These findings were concerning for necrotizing fasciitis. The patient was taken emergently to the operating room where she underwent wide excision and debridement of skin, fat, fascia of the right groin and perineum totaling 30 x 15 x 8 cm. She was then transferred to the intensive care unit, intubated, and put on inotropic support.
She went back to the OR multiple times over the course of her hospital stay for further wound exploration, washout, debridement, and reconstruction. Anaerobic cultures grew Prevotella and Porphorymonas species. Her hospital stay was complicated by septic shock and acute respiratory distress syndrome (ARDS); however, she improved and was discharged to subacute rehabilitation on day 24.
Her most recent monthly surgery follow-up revealed a well-healing wound with no complaints from the patient.
Discussion
Necrotizing fasciitis, specifically Fournier's gangrene, is a monomicrobial or polymicrobial severe flesh-eating deep soft tissue infection of the perineum and genitals.1 This extremely life-threatening and rare necrotizing fasciitis of the perineum carries with it an extremely high mortality rate. Most commonly, Fournier's gangrene appears to have a preference for individuals with a history of diabetes and alcohol abuse. The age of the patient, advancement of the disease, delayed presentation to the ED, and sepsis all contribute to the overall high mortality.
Necrotizing fasciitis progressively destroys muscle fascia and subcutaneous fat as it spreads along the fascia, with the overlying tissue often appearing unaffected by this flesh-eating infection. As a result, this can be a difficult diagnosis to make.6 The infection may follow a subacute and progressive course or may explode rapidly over days with multi-system organ dysfunction. The British Journal of Surgery reports that the following classic physical exam findings are only present up to 25% of the time and occur later in the disease process. As such, relying on these signs for a diagnosis can be dangerous.3,4
- Skin necrosis
- Crepitus (subcutaneous emphysema)
- Cutaneous anesthesia
- Bullae
- Severe sepsis/septic shock
Common physical exam findings to help the clinician differentiate necrotizing fasciitis from cellulitis includes:
- Pain out of proportion to physical exam findings
- Absence of lymphangitis
- Indistinct margins of involvement
- Tenderness beyond the location of erythema
- Worsening infection despite antibiotic use4
LRINEC Score
A scoring system that is helpful in prognosticating, but not diagnosing, and often helps in aiding clinical decision-making has been the LRINEC score (Laboratory Risk Indicator in Necrotizing Fasciitis). This scoring system utilizes 6 laboratory components (c-reactive protein, white blood cell count, hemoglobin, serum sodium, serum creatinine, and plasma glucose) that are each given a score, and the total score will assess the risk of necrotizing fasciitis. A score of ≥ 6 in the original study was found to have a 96% negative predictive value and a 92% positive predictive value.3
However, the score does have a limited sensitivity, has not been validated, not useful in the early recognition of necrotizing fasciitis, and there are reported cases in the literature of necrotizing fasciitis with a LRINEC score of 0.3
While necrotizing fasciitis can present with the previously mentioned lab abnormalities, interpreting the score with caution and maintaining a high index of suspicion are keys to identification.
Plain radiographs can show subcutaneous emphysema; however, this finding is only highly specific to Clostridia species.5 CT is more sensitive but does lack specificity as multiple different disease processes can reveal fluid collections, tissue stranding, and gas formation.
If suspicion is high for necrotizing fasciitis, immediate surgical consultation is necessary, even without imaging, as the gold standard for the diagnosis is surgical intervention.
Categorizing Necrotizing Fasciitis
Necrotizing fasciitis is divided into groups based on the type of bacteria. Type 1 infections are polymicrobial in nature and consist of gram-negative organisms (Klebsiella, Escherichia coli, Proteus, Enterobacter, and Pseudomonas) and anaerobes (Clostridia species, Bacteroides, Fusobacterium, Peptostreptococcus, and Prevotella).3,7
Type 1 infections are the most common and are typically found in patients with diabetes mellitus, obesity, chronic liver disease, recent surgery, peripheral vascular disease, omphalitis, and immunosuppression, to name a few.3 The synergistic effect of the bacteria can result in fulminate gangrene, multi-system failure, and death.
Type 2 infections are monomicrobial in nature and often caused by Streptococci and/or Staphylococci. Type 2 infections are typically found in healthy younger patients with a history of surgery, burn, trauma, laceration, or intravenous drug use.3,7
Type 3 infections are caused by gram-negative bacteria, specifically marine organisms like Vibrio species. These types of infections often occur after a break in the skin or an open wound is exposed to either saltwater or freshwater.3,7
Treatment
Antibiotic therapy should be broad to cover activity against gram-negative, gram-positive, and anaerobic bacteria. A commonly used acceptable regimen for the emergency physician will include broad spectrum coverage for gram positives, gram negatives, and anaerobes (vancomycin + piperacillin/tazobactam + clindamycin). After the results of gram stain, culture, and sensitivity, the antibiotic coverage can then be narrowed.
Summary
For the clinician, having a high index of clinical suspicion, prompt recognition, initiating broad-spectrum antibiotics early, and immediate surgical consultation are of paramount importance in potentially saving a life. Despite aggressive treatment, the mortality rate still ranges from 12-45%, and without surgery, 100%.2
Case Conclusion
This case report presents a patient diagnosed with Fournier's gangrene who received prompt treatment and surgical intervention and endured a complicated hospital stay, including septic shock and ARDS; however, she made a complete recovery.
References
1. Ahmed E. Fournier’s Gangrene: A Case Report. IJSR. 2016;5(1):925-926.
2. Arkoubi A, Sajad S. Fournier’s Gangrene-Case Report and a Brief Review. J Pakistan Derm. 2015;25(1):44-51.
3. Santistevan J. Necrotizing Fasciitis: Pearls and Pitfalls. emDOCS. Oct. 22, 2015.
4. Goh T, Goh L, Ang C, Wong C. Early diagnosis of necrotizing fasciitis. Br J Surg. 2014;101(1):e119-125.
5. Hakkarainen T, Kopari N, Pham T, Evans H. Necrotizing soft tissue infections: Review and current concepts in treatment, systems of care, and outcomes. Curr Probl Surg. 2014;51(8):344-362.
6. Stevens D, Baddour L. Necrotizing soft tissue infections. UpToDate. August 04, 2016.
7. Phan H, Cocanour C. Necrotizing soft tissue infections in the intensive care unit. Crit Care Med. 2010;38(9):S460-S468.