The magic of the modified Valsalva maneuver in cardioverting certain dysrhythmias is not without its own risks.
Supraventricular tachycardias (SVTs) are a diverse group of dysrhythmias that prompt patients to seek emergency care because of palpitations. The "Modified Valsalva Maneuver" has recently been reported to be a safe method of terminating a subset of these cases. Here we present the case of a 47-year-old female who arrived at the ED in a hemodynamically stable atrioventricular nodal reentry tachycardia (AVNRT). She was cardioverted utilizing the modified Valsalva maneuver, which was complicated by a period of non-sustained ventricular tachycardia (NSVT).
Background
The term supraventricular tachycardia is a catch-all phrase that refers to any rapid dysrhythmia that originates from a source superior to the ventricle. This includes atrial sources such as flutter and atrial fibrillation. More recently the term has come to colloquially refer more to atrioventricular reciprocating tachycardia (AVRT) such as that resulting from Wolff-Parkinson-White (WPW) and AVNRT.1 These rhythms alone rarely cause significant hemodynamic compromise as they most frequently occur in younger patients without structural heart disease, but they can certainly cause symptomatic palpitations, which is usually the presenting complaint.2 In the rare cases of hypotension, altered mentation, or other findings consistent with hemodynamic instability, electrical cardioversion is the appropriate initial therapy. However, for most patients, there are a variety of less invasive modalities. Vagal stimulation has long been an accepted first-line therapy for breaking supraventricular tachycardias in hemodynamically stable patients and the recent publication of the REVERT trial3 has led to increased awareness of the modified Valsalva maneuver as an effective intervention for terminating these dysrhythmias.
Case
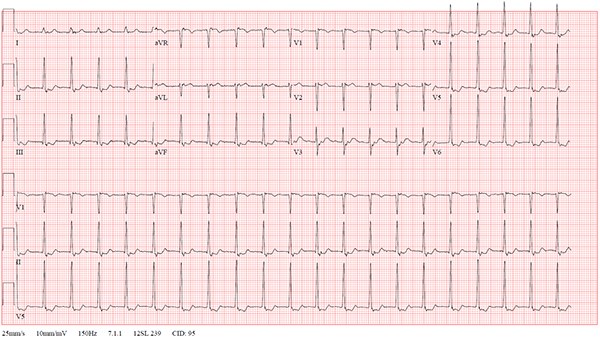
A 47-year-old female with a medical history only significant for recurrent SVT previously responsive to vagal maneuvers presented to the ED with a chief complaint of a rash (diagnosed as shingles). While driving to the hospital she developed (presumably unrelated) palpitations. EKG on arrival revealed a narrow complex tachycardia with a rate of 123 with retrograde P-waves consistent with AVNRT (Figure 1). The patient noted mild discomfort and palpitations but had normal blood pressure and no other concerning findings. The patient was placed on the cardiac monitor and cardioversion was attempted utilizing the modified Valsalva maneuver as described by Appelboam, et al.3 The procedure initially appeared successful, with a brief pause consistent with AV nodal blockade, but patient then developed non-sustained monomorphic ventricular tachycardia for a total of 10 beats, followed by a brief junctional escape rhythm, then resumption of AVNRT (Figure 2). Given this more malignant dysrhythmia, IV access was established, laboratory studies were sent, and the patient was attached to a defibrillator and planned for admission. A vagal maneuver was then attempted, this time a simple Valsalva without leg-raise modifications, and the patient was successfully cardioverted to sinus rhythm without additional incident (Figure 3). Blood work was unremarkable with normal electrolytes, troponin, and thyroid function, and she was admitted overnight for cardiology evaluation. Subsequent testing during admission was notable for peak Troponin I of 0.10 ng/mL several hours after the event, but there were no further significant dysrhythmias noted on telemetry. The patient’s previous records were obtained, including an echocardiogram that did not show evidence of hypertrophic cardiomyopathy. The patient was offered an ablation procedure but elected to follow up with her cardiologist and has had no further visits within our hospital system.
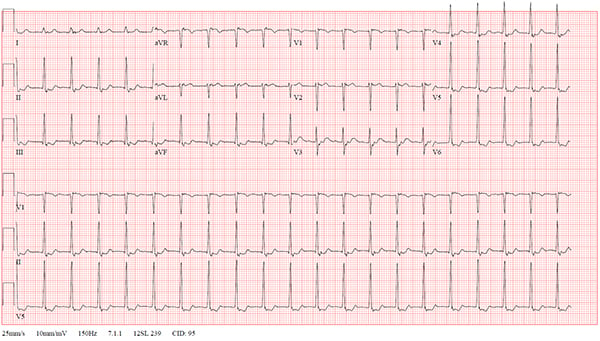
Figure 1. Initial EKG, narrow complex tachycardia with rate of 123 bmp, notable for retrograde P-waves buried in the ST segment
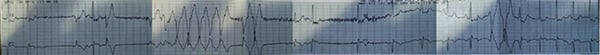
Figure 2. Rhythm strip immediately post cardioversion, as captured by telemetry monitor
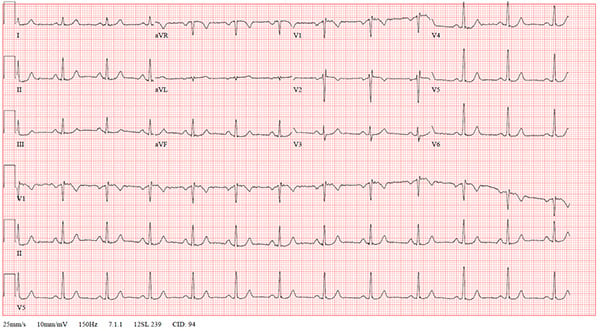
Figure 3. EKG after second (successful) cardioversion; patient remained in this rhythm for the rest of her hospital course
Discussion
Symptomatic supraventricular tachycardias (SVTs) are a common phenomenon, with a documented incidence of 35 cases per 100,000 people per year.4 Vagal maneuvers, including carotid massage, diving response, and Valsalva, previously have been used, with success rates from as low as 6% to a high of 54%.1 The mechanism of vagal response is likely due to post-synaptic innervation of the atrioventricular node via parasympathetic ganglion in the epicardium.5 While not always successful, the procedure is generally very well tolerated and there rarely adverse events. There are a limited number of case reports noting malignant dysrhythmias after vagal stimulation, and only 2 well-documented occurrences found through a search of the literature after treatment for SVT, neither of which resulted in any permanent harm.6,7
The modified Valsalva maneuver as first introduced by Appelboam, et al., in 2013 adds a period of passive leg raise after a “standardized strain” to further increase venous return. In theory this leads to stronger vagal stimulation and should increase the success rate of the procedure (indeed, in their paper cardioversion rate with the new technique was 43% vs 17% in the control group). However, this perhaps raises concerns that the vagal nerve may be overstimulated. While the rate of adverse effects in the original paper was not significantly different between the 2 groups (and most events were minor, such as mild nausea or transient muscle soreness from straining), the treatment group had 5 “electrograph captured events” (which were not further elucidated) vs 0 in the control group (no P value reported). Despite these concerns, the rate of significant adverse events with any form of vagal maneuver remains extremely low, and they should remain the first-line therapy in younger patients who are hemodynamically stable, per AHA class 1 recommendations.8 Exercise caution, however: Despite the appearance of stability, patients presenting with symptomatic SVT have, by definition, abnormal electrical conductivity through the heart and should always be treated with an appropriate level of caution.
Conclusion
While the modified Valsalva maneuver offers a simple, effective, minimally invasive, and overall very safe option for the treatment of supraventricular tachycardias, it is important to remember that the procedure alters the electrical conduction pathway through the atrioventricular node via vagal mediation. Strongly consider appropriate precautions, such as establishing IV access and placing defibrillator pads prior to attempting the procedure, in case a more malignant dysrhythmia develops, as it did in this case.
References
- Sohinki D, Obel OA. Current trends in supraventricular tachycardia management. Ochsner J. 2014;14(4):586-595.
- Colucci RA, Silver MJ, Shubrook J. Common types of supraventricular tachycardia: diagnosis and management. Am Fam Physician. 2010;82(8):942-952.
- Appelboam A, Reuben A, Mann C, et al. Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): a randomised controlled trial. Lancet. 2015;386(10005):1747-1753.
- Medi C, Kalman JM, Freedman SB. Supraventricular tachycardia. Med J Aust. 2009;190(5):255-260.
- Coote JH. Myths and realities of the cardiac vagus. J Physiol. 2013;591( 17):4073-4085.
- de Alencar Neto JN. Non-sustained polymorphic ventricular tachycardia following modified Valsalva maneuver: a case report. Case Reports: Open Access. 2017;2(101):1-4.
- De Mattia L, Brieda M, Del Bianco F, Dametto E, Nicolosi GL. Polymorphic ventricular tachycardia induced by Valsalva manoeuvre in a patient with paroxysmal supraventricular tachycardia. Europace. 2012;14(5):767-768.
- Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia. Circulation. 2016;133:e506-e574.