Although a rare diagnosis, ovarian torsion is an emergent cause of pelvic and abdominal pain.
As emergency department providers, we are primed to consider ovarian or adnexal torsion in our differential diagnosis in adult women presenting with pelvic pain, but are less likely to consider the diagnosis in pediatric populations. Although far less common in the pediatric population, occurring in approximately 4.9 per 100,000 women under the age of 201, ovarian torsion can occur in females of all ages, even fetuses and neonates, and remains a “can’t miss” diagnosis. Here, we present the case of an adolescent female who presented with fever and abdominal pain, and was initially misdiagnosed with spontaneous pelvic inflammatory disease, before the correct diagnosis of ovarian torsion was finally reached.
Case Presentation
An 11-year-old female with a history of obesity presented to the pediatric emergency department with left hip and left lower quadrant abdominal pain for 3 days. The patient reported that she fell on ice 4 days prior. She also endorsed nausea and vomiting. She had menarche 6 months prior and denied sexual activity. Vital signs included fever to 38.7°C (101.7° F), heart rate of 152, and blood pressure of 139/37. The physical exam revealed tenderness over the left lower quadrant without rebound or guarding, no bony tenderness to palpation over the greater trochanter or pelvis, and full range of motion of the hip. The patient ambulated with a steady gait. Labs were notable for white blood cell count of 25.5x109/L, CRP of 178.9 mg/L, normal urinalysis, and negative rapid urine gonorrhea and chlamydia.
Given the patient’s body habitus and her ill appearance, there was concern that an abdominal ultrasound would be insufficient to evaluate for intra-abdominal infection. A computed tomography of the abdomen and pelvis was performed, which showed a prominent cystic structure in the pelvis with a small to moderate amount of complex fluid. Subsequent formal transabdominal ultrasound demonstrated a cystic structure measuring 9.1 cm originating from the left ovary with low grade venous flow.
Gynecology was consulted and, given the patient’s fever and elevated inflammatory markers, admitted the patient with the presumed diagnosis of spontaneous pelvic inflammatory disease versus infected cyst. The patient continued to complain of left lower quadrant abdominal pain following admission despite initiation of broad spectrum antibiotics (cefotetan, doxycycline, and metronidazole). On hospital day 4, diagnostic laparoscopy revealed an enlarged and hemorrhagic appearing left ovary. The ovary and tube were torsed approximately 6-7 times. A paraovarian serous cyst was identified and drained. The ovary and fallopian tube were successfully de-torsed with improvement in color, and the patient was discharged with outpatient gynecology follow-up.
Discussion
Ovarian torsion is a surgical emergency and occurs when either the ovary or ovary and oviduct (termed adnexal torsion) twist on its ligamentous supports, resulting in congestion due to decreased venous return, decreased distal arterial blood flow, and ultimately ischemia and necrosis. The classic presentation of ovarian torsion is described as sudden onset, severe, colicky unilateral pain with guarding and adnexal enlargement on bimanual exam.15,8,3However, even within adult populations, ovarian torsion can be difficult to diagnose as not all patients follow this pattern. In a 15-year retrospective review, only slightly over half of patients reported sudden onset pain, and 44% reported crampy or colicky pain.2 Moreover, one-third of patients had only mild tenderness on abdominal exam, and 29% had no tenderness of pelvic exam. As a result, clinicians failed to consider ovarian torsion in the initial differential diagnosis in more than half of cases.
Within the pediatric population, a high clinical suspicion is necessary as atypical presentations are even more common. Although the majority of patients will present with abdominal pain, nausea, and vomiting, this presentation can occur with a variety of clinical conditions, and the differential diagnoses include appendicitis, pelvic inflammatory disease, gastroenteritis, and renal colic.3,4 In one retrospective cohort study comparing presentation of ovarian torsion in premenarchal and postmenarchal patients, premenarchal patients were more likely to present with restlessness (14.6% versus 0%), fever (9.8% versus 1%), palpable pelvic mass (9.8% versus 0%), and diffuse abdominal pain (29.3% vs. 7.2%).5 Similarly, a retrospective chart review of 83 cases reported higher rates of tachycardia in younger patients (37% versus 8%) and found that 20% of cases presented with a leukocytosis.6
Because pediatric patients are less likely to present with the typical symptoms associated with ovarian torsion, they are more likely to be initially misdiagnosed. In fact, compared to postmenarchal patients, a higher proportion of premenarchal patients were not evaluated by a gynecologist before surgery (12.2% compared with 0.5%)5. In another study, 38% of patients ultimately diagnosed with ovarian masses were originally diagnosed with appendicitis.7
Risk Factors
The primary risk factor for ovarian torsion is an enlarged ovary or ovarian mass greater than 4 cm. Risk of torsion correlates with size of ovarian mass, and more than 80% of adult patients with ovarian torsion had ovarian masses greater than 5 cm.8 Underlying ovarian abnormalities are a primary risk factor for the development of ovarian torsion in pediatric patients as well.3,4 Due to hormone stimulation, there is a known increase in functional ovarian cysts around the fetal period, first year of life, and menarche. In fact, up to 20% of females have multicystic and enlarged ovaries at menarche.3 However, ovarian torsion can occur in patients with no underlying pathology and, compared with older women, pediatric and adolescent patients ultimately diagnosed with torsion are more likely to have normal ovaries. In a 22-year retrospective chart review of pediatric patients, only 42% of patients with torsion presented with an ovarian mass or calcification, the mean size of which was 5.5 x 6.5 cm.4 For example, in one retrospective review, slightly less than 50% (10/22) of girls experiencing torsion had normal ovaries.9 Of interest, in both adult and pediatric patients, malignancy is a rare cause of ovarian torsion.2,3,4 Additionally, in both adult and pediatric populations, ovarian torsion occurs more commonly on the right than on the left.4,6,10 This may occur because right utero-ovarian ligament is longer, because of the presence of the sigmoid colon on the left, or because physicians are more likely to work up right-sided abdominal pain due to concern for appendicitis.
Diagnostic Imaging
In both adult and pediatric populations, the pelvic transvaginal ultrasound with doppler is the preferred diagnostic test. Findings on ultrasound can include an edematous, heterogeneous ovary, multiple small follicles (due to displacement by edema), and an enlarged ovarian or tubal cyst or mass. While it is common practice to obtain a transvaginal ultrasound in adult patients, transvaginal ultrasound is not appropriate for pediatric patients who are not sexually active. However, there is some data to suggest a transabdominal ultrasound may be sufficient. In Ashwal et. al., there were similar rates of ultrasound findings consistent with ovarian torsion in premenarchal patients, who exclusively had transabdominal ultrasounds performed, and postmenarchal patients, of whom 65% had a transvaginal ultrasound in addition to a transabdominal ultrasound. In pediatric patients, the most common finding is an enlarged ovary or an echogenic mass without visualization of the ovary.3,5
Regardless of modality, doppler can aid in the diagnosis of ovarian torsion if absent. However, the presence of normal arterial or venous doppler flow does not rule out ovarian torsion. The estimated sensitivity of doppler flow ranges from 43% to 92% and specificity of 100% to 97%, but data is inconsistent within pediatric populations.11,12 In one pediatric review, 62% of torsed ovaries had arterial or venous flow on doppler sonography.6 By comparison, in another review, 66% of patients had decreased or absent flow.2 And in Ashwal et. al., 53% of premenarchal and 63% of postmenarchal patients had either absent venous or arterial doppler flow.
The “whirlpool sign,” the ovarian vessels visualized wrapping around a central axis, is another ultrasound finding that is highly sensitive if present.8 In Ashwal et. al., 10% of patients had a positive whirlpool sign (two patients in the premenarchal group and 13 in the postmenarchal group).
Although not the gold standard, ultrasound is a helpful tool in the evaluation of ovarian torsion. If equivocal, MRI can be helpful in diagnosing ovarian torsion, as it can demonstrate components of a mass in more detail.8 Direct visualization is the only way to definitively make the diagnosis of ovarian torsion.8
What is Spontaneous PID?
In this case, the admitting diagnosis was spontaneous pelvic inflammatory disease (PID), a rare diagnosis. Following a literature review, we were only able to identify 14 case reports of spontaneous PID in the English language. Spontaneous PID in virginal patients is a polymicrobial infection, and is hypothesized to occur from bacterial seeding from bowel or ascension from the vagina. Hypothesized risk factors for spontaneous PID include obesity, constipation, chronic UTIs, poor hygiene, and cervical ectopy.13
One case describes an 11-year-old female with acute onset abdominal pain in the right lower quadrant associated with nausea and vomiting. She had a leukocytosis to 32.8 x 109/L, and an ultrasound showed a tubular structure in the right lower quadrant and moderate fluid in the pelvis. She was taken to the operating room with a presumptive diagnosis of appendicitis. However, on laparoscopy a large amount of purulent fluid in pelvis and posterior cul-de-sac were seen with an erythematous uterus and normal appendix. Pelvic fluid microscopy showed numerous polymorphonuclear leukocytes, but no growth of aerobic or anaerobic bacterial culture, and urine gonorrhea and chlamydia cultures were negative.
In another case report, a 13-year-old patient presented with abdominal pain, fever, and a cystic mass in the right lower quadrant. On laparoscopy she was diagnosed with a right pyosalpinx. After incision, purulent liquid was visualized, which ultimately grew E. coli.14
Despite these case reports, spontaneous PID is rare and poorly understood. However, it highlights that PID should be thought of as a polymicrobial disease, and that negative gonorrhea and chlamydia tests do not rule out PID.
Case Resolution
Two months following discharge, the patient was seen in a gynecology clinic for follow-up. The patient was asymptomatic at that time. Repeat ultrasound demonstrated a 4.8 cm complex cyst that was mostly cystic with solid components, likely representing residual clot from torsion. On a repeat visit four months after discharge, the patient remained asymptomatic. A repeat ultrasound was planned, and the patient has had no further follow-up visits in our system.

Image 1: CT scan of abdomen and pelvis demonstrating a prominent cystic structure in the pelvis and a moderate amount of complex fluid in the pelvis concerning for a ruptured follicle or corpus luteum, ovarian torsion, or neoplastic process.
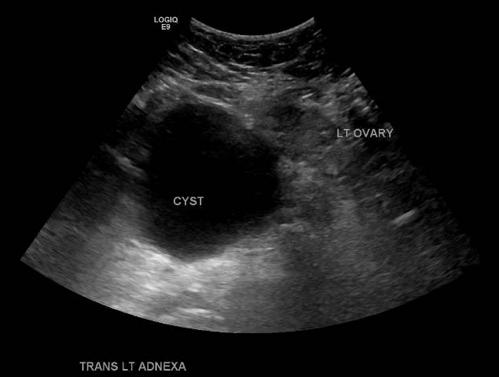
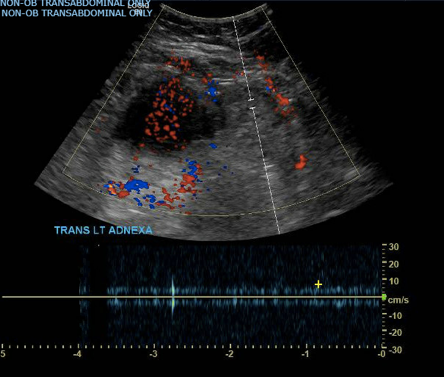
Image 2 and 3: Transabdominal ultrasound of the pelvis measuring 9.1 cm originating from the left ovary with low-grade venous flow.
References
- Guthrie BD, Adler MD, Powell EC. Incidence and trends of pediatric ovarian torsion hospitalizations in the United States, 2000-2006. Pediatrics. 2010;125(3):532-538. doi:10.1542/peds.2009-1360
- Houry D, Abbott JT. Ovarian torsion: A fifteen-year review. Ann Emerg Med. 2001;38(2):156-159. doi:10.1067/mem.2001.114303
- Cass DL. Ovarian torsion. Semin Pediatr Surg. 2005;14(2):86-92. doi:10.1053/j.sempedsurg.2005.01.003
- Beaunoyer M, Chapdelaine J, Bouchard S, Ouimet A. Asynchronous bilateral ovarian torsion. J Pediatr Surg. 2004;39(5):746-749. doi:10.1016/j.jpedsurg.2004.01.037
- Ashwal E, Hiersch L, Krissi H, et al. Characteristics and Management of Ovarian Torsion in Premenarchal Compared With Postmenarchal Patients. Obstet Gynecol. 2015;126(3):514-520. doi:10.1097/AOG.0000000000000995
- Rossi BV, Ference EH, Zurakowski D, et al. The clinical presentation and surgical management of adnexal torsion in the pediatric and adolescent population. J Pediatr Adolesc Gynecol. 2012;25(2):109-113. doi:10.1016/j.jpag.2011.10.006
- Pomeranz AJ, Sabnis S. Misdiagnoses of ovarian masses in children and adolescents. Pediatric Emergency Care. 2004;20(3):172-174. DOI: 10.1097/01.pec.0000117925.65522.e8.
- Huang C, Hong MK, Ding DC. A review of ovary torsion. Ci Ji Yi Xue Za Zhi. 2017;29(3):143-147. doi:10.4103/tcmj.tcmj_55_17
- Anders JF, Powell EC. Urgency of evaluation and outcome of acute ovarian torsion in pediatric patients. Arch Pediatr Adolesc Med. 2005 Jun;159(6):532-5. doi:10.1001/archpedi.159.6.532.
- Huchon C, Fauconnier A. Adnexal torsion: a literature review. Eur J Obstet Gynecol Reprod Biol. 2010;150(1):8-12. doi:10.1016/j.ejogrb.2010.02.006
- Nizar K, Deutsch M, Filmer S, Weizman B, Beloosesky R, Weiner Z. Doppler studies of the ovarian venous blood flow in the diagnosis of adnexal torsion. J Clin Ultrasound. 2009;37(8):436-439. doi:10.1002/jcu.20621
- Bar-On S, Mashiach R, Stockheim D, et al. Emergency laparoscopy for suspected ovarian torsion: are we too hasty to operate?. Fertil Steril. 2010;93(6):2012-2015. doi:10.1016/j.fertnstert.2008.12.022
- Kielly M, Jamieson MA. Pelvic inflammatory disease in virginal adolescent females without tubo-ovarian abscess. J Pediatr Adolesc Gynecol. 2014;27(1):e5-e7. doi:10.1016/j.jpag.2013.04.012
- Hornemann A, von Koschitzky H, Bohlmann MK, Hornung D, Diedrich K, Taffazoli K. Isolated pyosalpinx in a 13-year-old virgin. Fertil Steril. 2009;91(6):. doi:10.1016/j.fertnstert.2008.12.143
- Hang, Bophal Sarha. “Section 11: Obstetrics and Gynecology .” Tintinalli's Emergency Medicine, edited by Judith Tintinalli et al., 8th ed., McGraw Hill Education, New York, NY, 2016, p. 628



