Can you distinguish between an abnormal EKG and a cardiac device malfunction at a glance, recall common pacer codes, or identify pacemaker problems on an X-ray?
As the use of cardiac devices increases,1-2 emergency physicians must know how to manage not only patients who may need a pacemaker, but also those who present to the ED with a device already implanted. This article summarizes the indications for pacemaker insertion, evaluating a pacemaker on a chest X-ray, understanding pacer codes, interpreting normal and abnormal EKG findings with paced rhythms, and pacer malfunctions.
Indications for Pacemaker Insertion
Some of the Class I indications for pacemaker insertion per the 2012 ACCF/AHA/HRS guidelines3 include:
- Symptomatic sinus bradycardia
- Symptomatic chronotropic incompetence (failure to achieve 85% of age-predicted maximal heart rate during formal or informal stress test or inability to mount age appropriate heart rate during activities of daily living)
- Third-degree AV block
- Mobitz Type II second-degree AV block
- Recurrent syncope caused by spontaneously occurring carotid sinus stimulation and carotid sinus pressure that induces ventricular asystole of > 3 seconds
- For sustained pause dependent VT, with or without QT prolongation
- CHF with electromechanical ventricular dyssynchrony
Complications from Implantation
Although relatively rare, complications from pacemaker implantation typically occur within the first 6 weeks of placement and include:
- Infection
- Venous thrombosis of the upper extremity
- Superior vena cava syndrome
- Hemothorax
- Pneumothorax
- Pocket hematoma (bleeding associated with facial plane dissection for pocket creation)
Imaging
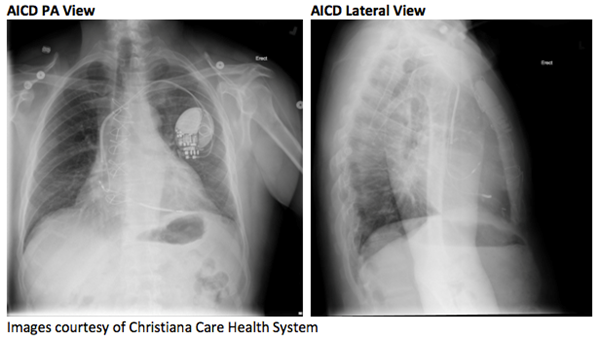
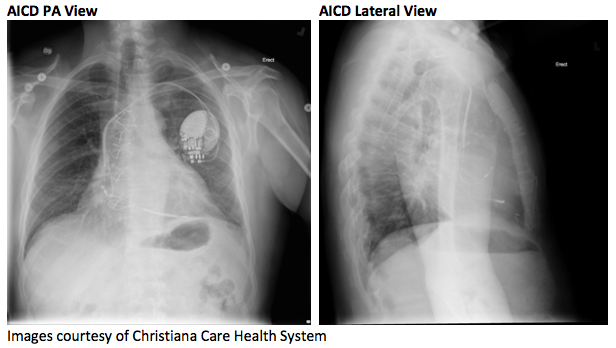
All cardiac pacemakers consist of a pulse generator and at least 1 lead connecting the generator to the myocardium. A chest x-ray should be obtained to evaluate for:
- Manufacturer code, which is found on pulse generator
- Compare pulse generator location with a prior CXR if available
- Leads (number, location, and continuity)
- A common fracture site is between the first rib and the clavicle
- AICD will have a thick coil that differentiates it from a pacemaker (as seen in AICD PA and Lateral Views)
Here’s what to look for on each view:
• The J portion of the right atrial lead will be medial.
• Right ventricular leads will point downward with the tip between the left edge of the vertebral column and the cardiac apex.
• Right atrial lead has a J-shaped appearance as it enters the right atrium and curves upward and anteriorly into the right atrial appendage.
• Right ventricular lead will course anteriorly and caudally.
• Leads placed in the left ventricle or coronary sinus should course posteriorly.
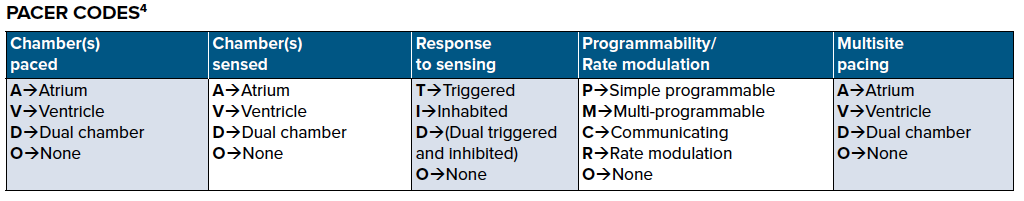
Pacer codes describe the function of the pacemaker. There is a 5-position code, of which the first 3 letters are the most relevant to the EM physician. The following are examples of typical codes:
VOO: The ventricle is paced asynchronously.
• Ventricle will be paced regardless of native cardiac activity.
VVI: The ventricle is paced and sensed.
• Ventricle is paced at a set rate.
• Pacing is inhibited if pacer senses intrinsic ventricular activity.
DDD: Both the atria and ventricle are paced and sensed.
• The pacemaker will either trigger or inhibit pacing based on whether it senses native cardiac activity.
• Atrial pacing is inhibited if a native atrial beat is sensed.
• Ventricular pacing is inhibited if a native ventricular beat is sensed.
• The pacer will trigger a ventricular beat if it senses an atrial beat (either paced or native) and there is no intrinsic ventricular beat within a programmed amount of time.
Normal ECG Findings with Pacemakers
- Pacing spikes are usually visible on the EKG.
- Spikes before P waves indicate atrial pacing.
- Spikes before QRS complexes indicate ventricular pacing.
- Spikes before both P waves and QRS complexes indicate dual chamber pacing.
- Atrial pacing
- Usually implanted in the right atrial appendage
- Typically results in P waves with normal morphology
- Single ventricle pacing
- Usually implanted in the apex of the right ventricle
- Typically results in an abnormal but predictable depolarization pattern that mimics a LBBB in the limb leads and anteroseptal precordial leads
- The major difference between an intrinsic LBBB and a paced rhythm is that the QRS will almost always be negative in V5-V6 with a paced rhythm.
- Pacing from the apex also often leads to left axis deviation.
-
-
- The presence of right axis deviation suggests that the pacing leads are implanted in the right ventricular outflow tract
- Epicardial pacing leads are sometimes placed over the left ventricle leading to a RBBB
- New RBBB pattern from prior suggests lead displacement
-
- Biventricular pacing
- Typically results in narrower QRS than with single ventricular pacing
- There will often be a dominant R wave in V1 +/- V2
Ischemia in Paced Rhythms
As with an intrinsic LBBB, ventricular pacing results in depolarization and repolarization abnormalities that can confound the EKG’s ability to detect an AMI and/or other findings concerning for ACS. In general, evaluate a paced EKG for ischemia as you would a LBBB.
Sgarbossa et al.5 found that concordant STE > 1 mm had the highest specificity (94%) for AMI in paced rhythms.
Maloy et al.6 showed that discordant STE > 5 mm had a 99% specificity for AMI. It’s important to note there were no cases in this study with STE > 1 mm. There are no studies applying the Modified Sgarbossa criteria to paced rhythms.
PEARL: The Sgarbossa criteria are specific but not sensitive for AMI, so the absence of these findings does not rule out an AMI.
Pacemaker Malfunctions
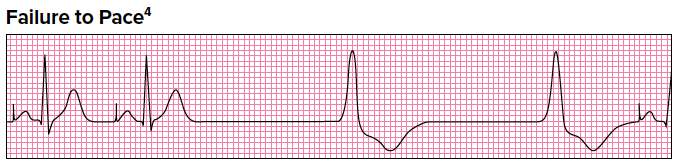
General Features
• Paced stimulus is not generated when expected
EKG Features
• Decreased or absent pacemaker spikes
Clinical Significance
• Causes: Oversensing (most common), lead fracture, or insulation defect
• Oversensing: Pacing is inhibited by non-cardiac activity (eg, skeletal muscle activity) inappropriately recognized as native cardiac activity
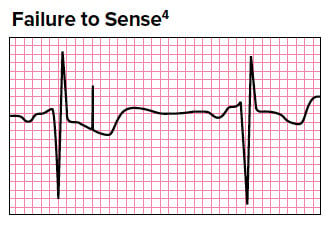
General Features
• Sensing refers to the pacer’s ability to recognize native cardiac beats
• Pacemaker fails to sense native cardiac activity → asynchronous pacing
EKG Features
• Pacing spikes within QRS complexes
Clinical Significance
• Causes: Lead insulation break, new intrinsic bundle branch block, electrolyte abnormalities, and Class IC antidysrhythmics (eg, flecainide)

General Features
• Delivery of pacing stimulus without subsequent myocardial depolarization
EKG Features
• Absence of depolarization after pacing spikes
Clinical Significance
• Functional etiologies include electrode displacement and wire fracture
• Pathologic etiologies include ischemia/infarct and electrolyte abnormalities (especially hyperkalemia)
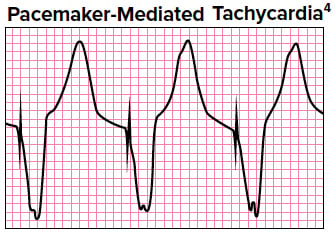
General Features
• Re-entry tachycardia with antegrade conduction through the pacemaker and retrograde conduction through AV node
• Only occurs with dual chamber pacemakers
EKG Features
Paced wide complex tachycardia (may see retrograde P-waves)
Clinical Significance
• Rate limited by pacemaker programming
• Treat with adenosine or magnet
Summary
It’s important to gain a solid understanding of pacemaker evaluation and management in the ED. Emergency physicians should have a low threshold to obtain further information from device interrogation and involve Cardiology when indicated.
References
1. Greenspon AJ, Patel J, Lau E, et al. Trends in Permanent Pacemaker Implantation in the United States 1993-2009: Increasing Complexity of Patients and Procedures. J Am Coll Cardiol. 2012;59(13):SE703.
2. Uslan DZ, Tieyjeh IM, Baddour LM, Friedman PA, Stoner SM, St Sauver JL, Hayes DL. Temporal Trends in Permanent Pacemaker Implantation: A Population-Based Cohort Study. Circulation. 2018;114(S18):832.
3. Writing Group. 2012 ACCF/AHA/HRS Focused Updated Incorporated into the ACCF/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities. J Am Coll Cardiol. 2013;61(3):e6-e75.
4. Berberian JG. EMRA EKG Guide. 1st ed. Dallas, TX: Emergency Medicine Residents’ Association; 2017.
5. Sgarbossa EB, Pinski SL, Gates KB, Wagner GS, The GUSTO-1 Investigators. Early electrocardiographic diagnosis of acute myocardial infarction in the presence of ventricular paced rhythm. J Am Coll Cardiol. 1996;77(5):423-424.
6. Maloy KR, Bhat R, Davis J, Reed K, Morrissey R. Sgarbossa Criteria Are Highly Specific for Acute Myocardial Infarction with Pacemakers. West J Emerg Med. 2010;11(4):354-357.