Ventricular pacemakers typically cause a delay in repolarization of the ventricles; this in turn can obscure the usual ST changes seen in an acute myocardial infarction.
Left bundle branch blocks (LBBBs) are commonly seen in ventricular paced rhythms and require further evaluation of acute ischemic events using the widely recognized Sgarbossa criteria.
We present a patient with a biventricular pacemaker and chest pains. His EKG findings show ST segment elevations in anterior and lateral leads, concerning for an anterolateral STEMI.
Case
Our patient, a 93-year-old male with a complex cardiac history including complete heart block with biventricular pacemaker and atrial fibrillation on clopidogrel, presented to a community emergency department with symptoms of constant left-sided non radiating chest pressure that awakened the patient from sleep. He found himself in cold sweats at that time, prompting emergency department evaluation.
On physical exam, his vital signs were significant for hypertension of 148/100, otherwise unremarkable. There were no murmurs, asymmetric pulses, chest wall tenderness, or crepitus. The initial EKG was concerning for a ventricularly paced rhythm with a rate of 70 bpm and ST elevations in lateral and anterior leads (Image 1).
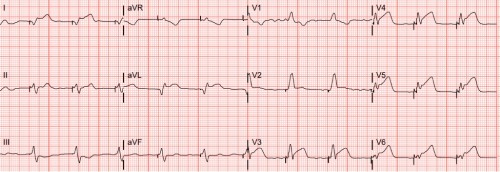
Image 1: EKG
These were new changes when compared to the last documented EKG. The cardiology team was contacted prior to activating the cath lab, as the patient had a biventricular pacemaker. Upon discussing the patient’s case with the interventional cardiologist, the decision was made to activate the cath lab. The patient was given aspirin and ticagrelorand transferred to Akron City for heart catheterization.
The patient was found to have total occlusion of the mid left anterior descending artery, for which he received balloon angioplasty and PCI (Images 2 and 3).
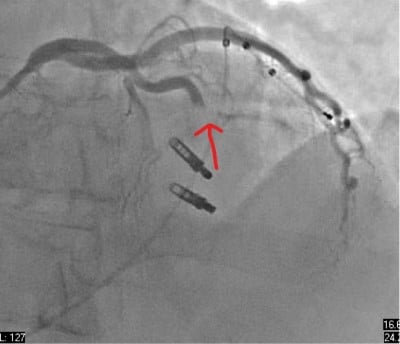
Image 2 (above): Pre-balloon angioplasty and PCI

Image 3 (above): Post-balloon angioplasty and PCI
Discussion
Biventricular pacemakers are devices that stimulate both the right and left ventricle simultaneously, which can result in a range of abnormal baseline EKG morphology related to variations in impulse timing and lead placement. As such, it can be challenging to diagnose coronary-related ischemia in these patients.
There is limited literature on the sensitive and specific EKG changes for myocardial infarction in these patients.3However, depending on the location, some pacemakers can create left bundle branch morphology, allowing for the well-known and reliable Sgarbossa criteria and the modified Sgarbossa criteria to play a role in diagnostic evaluation. Several studies have validated both the Sgarbossa and modified Sgarbossa criteria in patients with RV pacemakers, and this may be the closest criteria that can be useful in evaluating patients with ventricularly paced rhythms.4
To review, the Sgarbossa criteria refers to:
1) ST-segment elevation >1 mm in the same direction as the QRS complex (concordant) in any lead
2) ST-segment depression >1 mm in the same direction as the QRS complex (concordant) in at least one chest lead (i.e., V1 to V6).
3) ST-segment elevation >5 mm in the opposite direction as the QRS complex (discordant)1
The modified Sgarbossa criteria has the same first and second rule, but the third is replaced by:
3) ST-elevation (mm) / S-wave amplitude (mm) ratio >0.25 (a measure of discordance) from the lead that generates the greatest ST-elevation/S-wave ratio2
Of these criteria, literature suggests only the third criteria of the original Sgarbossa (ST-segment elevation >5 mm discordant with the QRS complex) was highly specific and statistically significant in ventricular paced rhythms.6,7,8
Patients with ventricularly paced rhythms are at higher risk for poor outcomes due to the difficulty in diagnosing ischemia in this population. In addition, patients can have atypical presentations such as the absence of chest pain. Atypical presentations in conjunction with no current highly sensitive or specific EKG criteria for ischemia can lead to delayed intervention and overall greater morbidity and mortality in ventricularly paced patients,5 which highlights the relevance of judicious evaluation by ED providers. The Sgarbossa criteria can help more timely management in ventricularly paced patients and should not be limited to those with LBBB only.
The patient discussed in the case above had concordant ST-segment elevation of >1 mm in 1, aVL, V3 - V6. Despite placement of a biventricular pacemaker, the patient had classic ST-elevation in contiguous leads warning of ischemia, a highly unusual finding in the setting of a paced rhythm.
Overall, more studies need to be done to create sensitive and specific criteria for coronary-related ischemia in patients with biventricular pacemakers, but high clinical suspicion, changes in EKG, and early recognition can help with timely intervention for appropriate care.
Take-Home Points
• There is neither very good data nor scores to diagnose a STEMI from a paced ECG considering the sensitivity and specificity of Sgarbossa.
• Classic ST elevation pattern can be seen in ventricularly paced rhythms.
• Clinical suspicion may be more telling than the EKG in patients with biventricular paced rhythms.
References
- Sgarbossa EB, Pinski SL, Barbagelata MD, et al. Electrocardiographic Diagnosis of Evolving Acute Myocardial Infarction in the Presence of Left Bundle-Branch Block. N Engl J Med. 1996;334(8).
- Smith SW, Dodd KW, Henry TD, et al. Diagnosis of ST-Elevation Myocardial Infarction in the Presence of Left Bundle Branch Block with the ST-Elevation to S-Wave Ratio in a Modified Sgarbossa Rule. Annals of Emerg Med. 2012;60(6).
- Khawaja M, Thakker J, Kherallah R, Ye Y, Smith SW, Birnbaum Y. Diagnosis of Occlusion Myocardial Infarction in Patients with Left Bundle Branch Block and Paced Rhythms. Curr Cardiol Rep. 2021;23(12):187.
- Borovac JA, Orsolic A, Miric D, Glavas D. The use of Smith-modified Sgarbossa criteria to diagnose an extensive anterior acute myocardial infarction in a patient presenting with a left bundle branch block. J Electrocardiol. 2021 Jan-Feb;64:80-84.
- Rathore SS, Gersh BJ, Weinfurt KP, Oetgen WJ, Schulman KA, Solomon AJ. The role of reperfusion therapy in paced patients with acute myocardial infarction. Am Heart J. 2001 Sep;142(3):516-9.
- Sgarbossa EB, Pinski SL, Gates KB, Wagner GS. Early electrocardiographic diagnosis of acute myocardial infarction in the presence of ventricular paced rhythm. Am J Cardiol. 1996 Feb 15;77(5):423-4.
- Abraham AS, Vinson DR, Levis JT. ECG diagnosis: Acute myocardial infarction in a ventricular-paced rhythm. Perm J. 2019;23:19-001.
- Maloy KR, Bhat R, Davis J, Reed K, Morrissey R. Sgarbossa criteria are highly specific for acute myocardial infarction with pacemakers. West J Emerg Med. 2010 Sep;11(4):354-7.



