Critically ill pediatric patients can make physicians-in-training nervous - and that anxiety is heightened when it comes to a pediatric patient in respiratory distress. This article reviews the basics of managing the pediatric airway, which has key differences from the adult airway.
Case 1
A 2-year-old boy from Ecuador is brought into your community ED. The nurse quickly brings the child into the critical care bay because of respiratory distress and begins placing the child on a monitor. You note the child to have inspiratory stridor and to be tripoding. Oxygen saturation is 88% on room air, heart rate is 165, respiratory rate is 55, and auricular temperature is 39.0 C. You are unable to immediately obtain a history from the mother because of a language barrier. You ask the nurse to administer nebulized epinephrine while you grab the pediatric airway cart and contact the "on-call" anesthesiologist.
Case 2
A 4-year-old, fully vaccinated girl is brought in by her father because of an acute onset of cough and wheeze since this morning. In triage the patient is given albuterol and placed on a monitor. When you walk into the room, you observe a mildly tachypneic patient, with inspiratory stridor at rest and clear nasal discharge. On auscultation you hear diffuse wheeze. There are no other pertinent exam findings, but the dad tells you the patient gets frequent upper respiratory infections for which she sometimes requires albuterol. Your differential includes croup, early epiglottitis, foreign body, reactive airway disease and early retropharyngeal abscess. You order nebulized epinephrine along with a portable chest and neck X-ray. After albuterol and nebulized epinephrine, no change is noted on exam. The X-ray tech comes by to show you the image, and while you notice a possible foreign body the nurse calls you over for help.
Case 3
It is mid-December and a mother brings in her 6-month-old boy because of worsening respiratory distress and decreased energy and appetite over the past 3 days. His past medical history is significant for 34 weeks gestation, and a 2 day NICU stay. He has since been medically stable. The infant is placed on a monitor and his respiratory rate is 70, with an oxygen saturation of 86%, a heart rate of 180, and a temperature of 102.9 F. On exam, you note upper airway congestion, nasal flaring, subcostal retractions, abdominal breathing, and bilateral wheezing. Nasal suctioning only improves oxygen (O2) saturation to 88% with no change in work of breathing (WOB). You have the nurse start blow-by with no improvement in WOB or O2 saturation. The patient is administered nebulized albuterol, while IV access, blood cultures, and a portable chest X-ray are obtained. You instruct the nurse to give 20 cc/kg of fluids.
The Pediatric Airway
As emergency physicians-in-training, we can feel uncomfortable when caring for critically ill pediatric patients. This anxiety can be heightened when facing a pediatric patient in respiratory distress and a potentially difficult airway. This article will review some of the basics of the management of the pediatric airway (including anatomical differences, initial interventions, definitive airways, medication selection, ventilator settings, and difficult airways) in the hopes of somewhat lessening that anxiety.
The steps to the pediatric airway parallel that of an adult. Just as in adults, managing the pediatric airway requires a familiarization with the equipment and a stepwise approach that begins with assessment of airway patency followed by identifying an oxygenation or ventilation issue.
For the child in respiratory distress, initial interventions include low-flow oxygen delivery systems (< 10 L/min), such as a nasal cannula or simple oxygen mask. If the patient fails to respond, high-flow oxygen delivery systems, such as non-rebreathing mask with reservoir or high flow nasal cannula can be used.18 These modalities deliver oxygen but do not help with pressure support. If these interventions fail, initiation of noninvasive positive pressure ventilation via high-flow nasal cannula (HFNC), continuous positive airway pressure (CPAP), or bi-level positive airway pressure (BIPAP) should be attempted.
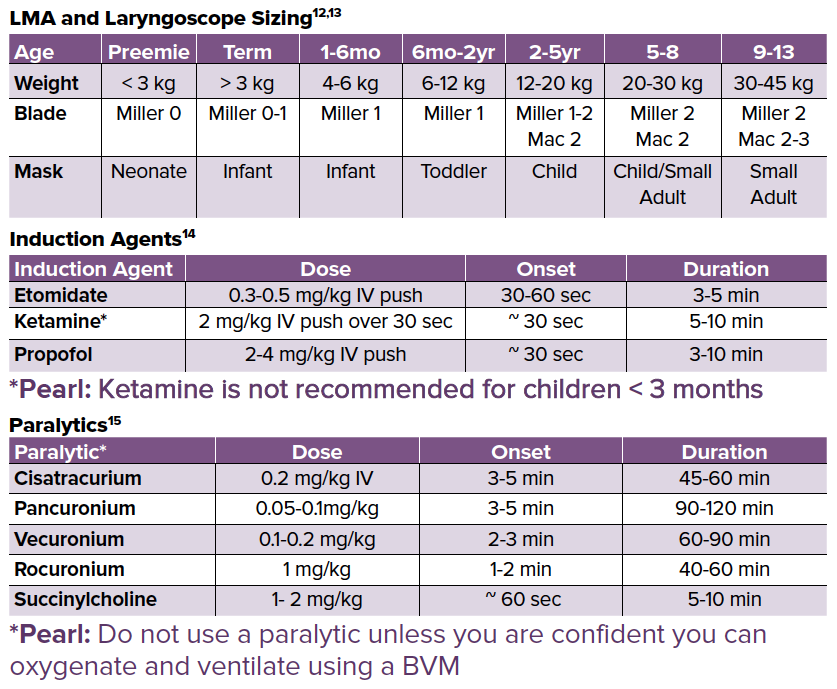
Finally, in patients with persistent respiratory distress despite these efforts, a definitive airway should be established. While supplies are gathered for the definitive airway, a bag-valve mask (BVM) can be used to bridge the patient. There are several options for invasive airways in the pediatric patient, including supraglottic airways (King tube, LMA, etc), endotracheal, or in some cases, nasopharyngeal intubation. As a last resort, needle-cric and jet ventilation in pediatrics under 8 years old or traditional cricothyroidotomy for those patients above 8 years old can be attempted.2
When attempting intubation in children, several anatomic factors can result in airway obstruction or can complicate the visualization of the vocal cords. Children younger than 2 years of age have large occiputs, causing neck flexion in the supine position, leading to tracheal obstruction and malalignment of the oropharynx with the larynx and vocal cords.1,10 The pediatric airway is also shorter, floppier, and narrower than in adults, making it more susceptible to kinking and obstruction.1 Children also have larger tongues relative to the size of their oropharynx, which increases the risk of obstruction and difficulty visualizing the cords.1,10 Furthermore, the epiglottis is floppier, making it difficult to manipulate in order to visualize vocal cords.1,10 There is also increased risk of right mainstem intubation due to the short tracheal distance leading to the right main bronchus.1
Even after successful maneuvering of the endotracheal tube (ETT) past the vocal cords, there may be difficulty passing the ETT further. This is because the narrowest portion of the pediatric airway is the cricoid cartilage, rather than the vocal cords in adults.1,10 If the ETT is difficult to pass, a smaller ETT must be attempted to avoid mucosal injury and airway edema, which can be exchanged via a bougie/gum elastic bougie, for example.
Besides anatomic differences, there are physiologic differences that impact the management of the pediatric airway. Pediatric patients have a higher oxygen demand and oxygen consumption. Combined with smaller airway volumes, the higher oxygen demand and consumption results in lower functional residual capacity and a smaller oxygen reserve.4 Additionally, abdominal distension, most commonly due to too much BVM ventilation prior to intubation, can lead to decreased functional residual capacity and O2 desaturation.4
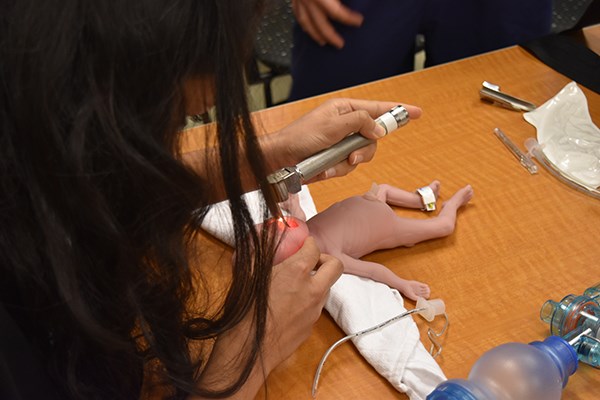
There are a number of techniques providers can utilize in order to optimize first-pass intubation rates. Placing a towel underneath the shoulders and using the head tilt-chin lift maneuver can overcome the neck flexion caused by the larger occiput, resulting in better oropharyngeal and laryngeal alignment, and reduce airway obstruction.1 It is important to avoid overextension, which may also result in airway obstruction due to the flexible trachea. In order to avoid airway obstruction when utilizing non-invasive airway adjuncts like BVM, as a result of the large pediatric tongue, it is important to open the mouth widely via the jaw thrust maneuver or by placing an oral or nasal airway.10 The jaw thrust maneuver can also be utilized to prevent the large pediatric tongue from obscuring your view of the airway. Additionally, a miller blade should preferentially be utilized in children < 2 years old to allow for better control of the floppy epiglottis and better view of the anterior pediatric airway.10
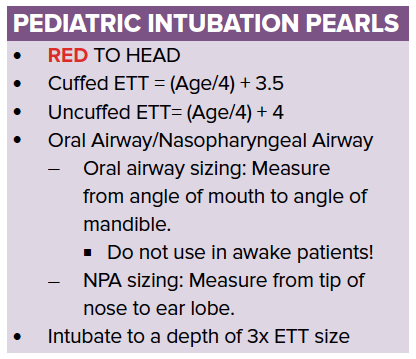
Set up for the pediatric airway is no different from the adult airway, except for the sizing of equipment. The Broselow tape is a useful adjunct, as it can be used to determine the size of equipment needed and the medication dosing. The Broselow tape is placed at the patient's head and is used to measure the length of the child, which correlates to the dosing and sizing of medication and equipment. Remember the mnemonic, RED to HEAD, which means to place the red color of the Broselow to the patients head, and then measure to the patient's heel.
Difficult Pediatric Airways
Management of the airway should always include preparation for possible difficulties. Familiarizing yourself with the location of the necessary equipment and a step-wise assessment of your equipment beforehand is essential. You should have yankauer suction, BVM attached to oxygen, a monitor that can measure end tidal CO2, multiple laryngoscope blade sizes with working lights, and multiple sizes of ETT with stylets. If using video laryngoscopy, the video should be tested prior to use.
There should also be airway adjuncts and supplies for difficult airways, including bougie, OPA, NPA, and scalpel. However, standard issue bougies do not fit most pediatric sized ET tubes; rather, a gum elastic bougie (GEB) should be used.18
Finally, the patient should have a working IV or IO line and the nurses should have appropriate medications and doses. If there is time, consent should be obtained and the ventilator set up.
If you attempt to intubate and fail, then the most experienced provider should be given the next attempt. After 1-2 failed attempts at securing an airway either via direct or video laryngoscopy, after you BVM to re-oxygenate, your next step can include utilization of a bougie/GEB or lighted stylet.18 However, an experienced provider should make the attempt, as GEB and lighted stylets are not routinely used in pediatrics.18 If that fails, you may be able to temporize with a supraglottic device until you can get the patient to a pediatric ENT or anesthesiologist. Care should be taken because supraglottic devices are contraindicated in epiglottitis.
Surgical Airway
The last line in a critically ill pediatric patient who has respiratory failure is cricothyroidotomy. Depending on the age, either needle cricothyroidotomy with jet ventilation in children < 8 years old (due to the smaller size of the cricoid membrane) or traditional cricothyroidotomy in children > 8 years old should be implemented.2 When attempting a needle cricothyroidotomy, be wary of the compressibility of the cricoid, as there is a larger risk of puncturing through to the esophagus compared to adults.1
Needle Cricothyroidotomy
To perform needle cricothyroidotomy, follow these steps:
- Identify the cricothyroid membrane, found inbetween thyroid and cricoid cartilage, and prepare a sterile field.
- Connect a 14 gauge needle to a syringe with 3-5 cc of sterile saline. Insert the needle and advance at a caudal angle while withdrawing until you see air bubbling, confirming placement.1
- Connect a 14 gauge to 3.0 ET tube adapter.
At this point the patient can be oxygenated but very poorly ventilated, with approximately 40-60 minutes max until a more definitive airway is necessary.
Post Intubation
Post-intubation steps are similar between pediatric and adult patients. Tube placement should be confirmed through auscultation of bilateral breath sounds, fogging of the ETT, and CO2 capnography. A gastric or nasogastric tube should be placed to decompress the stomach contents in order to reduce aspiration risk while improving expansion of the diaphragm and therefore, functional residual capacity. It is important to obtain post-intubation chest X-ray for tube confirmation; similar to adults, the tip of the tube should be 2 cm above the carina.8
After the tube placement is confirmed, the patient should be placed on a ventilator and sedation started. Below are some general guidelines for initial settings in the emergency department which can be modified based on patient needs.6,7
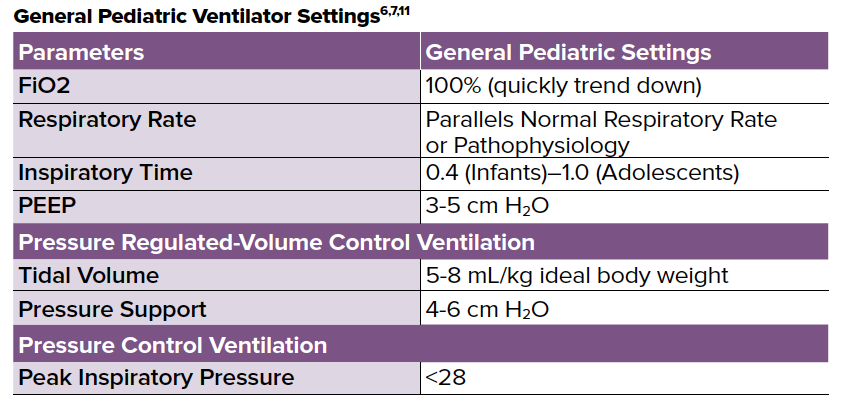
An important contrast between pediatric and adult basic ventilator settings is that pediatric patients are most often placed on pressure control setting due to the higher risk of ventilator associated barotrauma.6,7
After intubation and placement on a ventilator, then, based on the pathophysiology of the patient, a sedative and/or long acting paralytic may need to be initiated. Benzodiazepines like midazolam are commonly used in pediatric patients, as well as fentanyl or propofol. These can be used as either pushes or continuous infusions.9
Case 1 Continued
The on-call anesthesiologist is 10 minutes out. You are worried about epiglottitis and anticipate a difficult airway. You set up for emergent intubation with suction, BVM, 1.0 miller blade, and a cuffed 3.5/4.0 ETTs. As backup you have video laryngoscope, GEB and a 14 gauge needle with a 3.0 ET tube adapter for possible needle cricothyroidotomy. Suddenly the patient becomes unconscious and bradycardic to the 50s. CPR is initiated and oxygenation with a BVM is started. The O2 saturation remains in the 80s despite repositioning of the airway, verifying a tight face-mask seal and continued BVM use. When you attempt to visualize the cords during direct laryngoscopy, they are obstructed by a markedly swollen epiglottis. You attempt to intubate via video laryngoscope and GEB, but are unsuccessful. Given the situation, you perform a needle cricothyroidotomy and start jet-ventilation with successful improvement in O2 saturation. Anesthesia arrives and you aid in the successful nasal intubation of this patient via a flexible bronchoscope and 3.0 uncuffed ETT. You start a midazolam drip, send labs, start IV antibiotics and arrange for transfer to the nearest Pediatric Intensive Care Unit.
Case 2 Continued
You enter the exam room and see that the patient is grabbing at her neck and has no stridor. You start abdominal thrusts as she is unable to make sounds and is still responsive. Simultaneously, the nurse grabs the airway cart, Magill forceps, a 2.0 Mac blade, a 4.0/4.5 cuffed ET tube, a child BVM and the cricothyroidotomy tray. After placing the patient supine on the bed, she becomes unresponsive and you start CPR, while the nurse calls for help and contacts the on-call ENT resident. You visualize the airway and see a small round object in the trachea right below the vocal cords, which you cannot grab with the Magill forceps. You quickly decide to intubate, pushing the foreign body down into the right main bronchus, and then selectively intubate the left lung with improvement in ventilation and oxygenation via BVM. The patient is placed on a pressure regulated low tidal volume ventilator setting and transitioned with ENT to the operating room for rigid bronchoscopy with successful removal of the foreign body.
Case 3 Continued
The portable chest X-ray was unremarkable. You begin HFNC at 2 L/kg/ min, which brings the oxygen saturation to 88% and the patient continues to be tachypneic to 75.16 Given the severity of disease, you administer nebulized epinephrine with minimal improvement in WOB. The patient starts to fatigue and the O2 saturation falls back to 80% with a RR of 80 and HR of 175. Due to impending respiratory failure you intubate the patient with etomidate and rocuronium, using a Miller 1 and 3.5 cuffed ET tube. You start a midazolam drip and place the patient on a pressure control settings with FiO2 of 100% while awaiting transfer to PICU.
(Disclaimer: Cases are all fictional.)
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
References
Harless, J., Ramaiah, R., & Bhananker, S. M. (2014). Pediatric airway management. International journal of critical illness and injury science, 4(1), 65.
Roberts JR, Custalow CB, Thomsen TW, et al., editors. Roberts and Hedges’ clinical procedures in emergency medicine, 6th ed. Saunders: Philadelphia, 2013.
Katos, M. G., & Goldenberg, D. (2007). Emergency cricothyrotomy. Operative Techniques in Otolaryngology-Head and Neck Surgery, 18(2), 110-114.
Huang AS, Rutland L, Hajduk J, Jagannathan N (2016). Difficult airway management of children in ambulatory anesthesia: challenges and solutions, Ambulatory Anesthesia, 3, 37-45
Graciano, A. L., Tamburro, R., Thompson, A. E., Fiadjoe, J., Nadkarni, V. M., & Nishisaki, A. (2014). Incidence and associated factors of difficult tracheal intubations in pediatric ICUs: a report from National Emergency Airway Registry for Children: NEAR4KIDS. Intensive care medicine, 40(11), 1659-1669.
Pediatric acute respiratory distress syndrome: consensus recommendations from the Pediatric Acute Lung Injury Consensus Conference. Pediatric Acute Lung Injury Consensus Conference Group Pediatr Crit Care Med. 2015;16(5):428.
Rimensberger PC, Cheifetz IM. Ventilatory support in children with pediatric acute respiratory distress syndrome: proceedings from the Pediatric Acute Lung Injury Consensus Conference. Pediatric Acute Lung Injury Consensus Conference Group. Pediatr Crit Care Med. 2015;16(5 Suppl 1):S51.
Salem MR. Verification of endotracheal tube position. Anesthesiol Clin North America. 2001;19(4):813.
Kudchadkar SR, Easley RB, Brady KM, Yaster M. Pain and sedation management. In: Rogers' Textbook of Pediatric Intensive Care, 5th ed, Nichols DG, Shaffner DH (Eds), Wolters Kluwer, Philadelphia 2016. P.132.
Holm‐Knudsen, R. J., & Rasmussen, L. S. (2009). Paediatric airway management: basic aspects. Acta Anaesthesiologica Scandinavica, 53(1), 1-9.
Kneyber, M. C., De Luca, D., Calderini, E., Jarreau, P. H., Javouhey, E., Lopez-Herce, J., & Pons-Odena, M. (2017). Recommendations for mechanical ventilation of critically ill children from the Paediatric Mechanical Ventilation Consensus Conference (PEMVECC). Intensive care medicine, 43(12), 1764-1780.
Open Anestheisa. (2019). Pediatric Anesthesia. Retrieved April 1, 2019, from https://www.openanesthesia.org/pediatric_anesthesia_anesthesia_text
University of California, San Francisco Anesthesia (2007). Pediatric Pocket Reference Card. Retrieved April 1, 2019 from https://anesthesia.ucsf.edu/sites/anesthesia.ucsf.edu/files/wysiwyg/pdfs/PediRefCard.pdf
University of Chicago, Department of Pediatric Emergency Medicine (2013) Comer Emergency Department Clinical Guidelines: Rapid Sequence Intubation Pediatric Pearls. Retrieved April 1, 2019 from zhttps://pediatrics.uchicago.edu/sites/pediatrics.uchicago.edu/files/uploads/Rapid%20Sequence%20Intubation.RSI%202013.pdf
Agrawal, D., (2018). Rapid sequence intubation (RSI) outside of the operating room in children: Medications for sedation and paralysis. Post TW, ed. UpToDate. Waltham, MA: UpToDate Inc. Retrieved April 1, 2019 from https://www.uptodate.com
Mikalsen I, Davis P, and Oymar K High flow nasal cannula in children: a literature review. Scand J Trauma Resusc Emerg Med. 2016; 24: 93.
De Caen AR, Berg MD, Chameides L, et al. Part 12: Pediatric Advanced Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015; 132:S526.
King, C. Emergent endotracheal intubation. In: Textbook of Pediatric Emergency Procedures, Henretig, FM, King, C (Eds), Lippincott Williams & Wilkins, Philadelphia 1997. p.161.