Introduction
Intracranial abscesses are a rare pathology in which focal areas of brain parenchyma are necrotic secondary to an infectious agent, typically bacteria, with an incidence of 1,500-2,500 cases in the United States per year.1,3 The incidence in children is likely even less, and unfortunately there is very little data on specific pathology. While extremely rare, it should remain on the differential when evaluating children who present to the emergency department with fussiness, altered mental status, and headaches. Specifically in infants, head circumference measurements provide a useful objective measurement that could guide the clinician toward intracranial pathologies, such as a brain abscess, in an otherwise undifferentiated fussy infant.
In this case report, we will present a case of a 2-month-old male who presented with fussiness and increasing head circumference and was ultimately found to have an intracranial abscess. In this case review, we hope to highlight the importance of cranial circumference measurements in the emergency department while reviewing this rare pathology.
Case Report
The patient is a 2-month-old male, born at 37-weeks’ gestation via spontaneous vaginal delivery without complication, who presented to the pediatric ED with increased head circumference, fussiness, and progressively increasing vomiting over the past week. The mother reported that he had recently started daycare and had mild nasal congestion. She denied fevers, but did endorse an elevated temperature of 99.8 for which she administered acetaminophen. Mom reports the patient had not yet had his 2-month vaccinations, but received all recommended medications at birth.
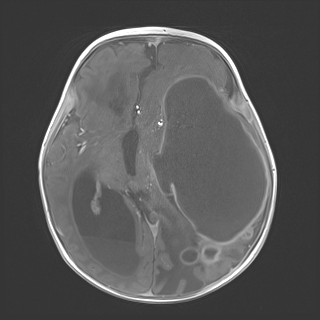
Vital signs were blood pressure 126/62, heart rate 149, respiratory rate 44, and pulse oximetry 100% on room air. On physical exam, the patient was irritable and had a bulging fontanelle with a large head circumference, 47 cm, greater than the 98th percentile. His previously recorded head circumference was 34.9 cm at birth, which was at the 63rd percentile (Figure 1). His pupils were 5 mm and equally reactive; however, he did have restriction of extraocular movements with a fixed downward gaze. He moved all four extremities equally. Skin exam was significant for an erythematous patch over the chest, consistent with a known birthmark. He had no bruising, abrasions, or lacerations concerning for trauma to his head. His heart and lung sounds were normal, and his abdomen was soft and nontender to palpation.
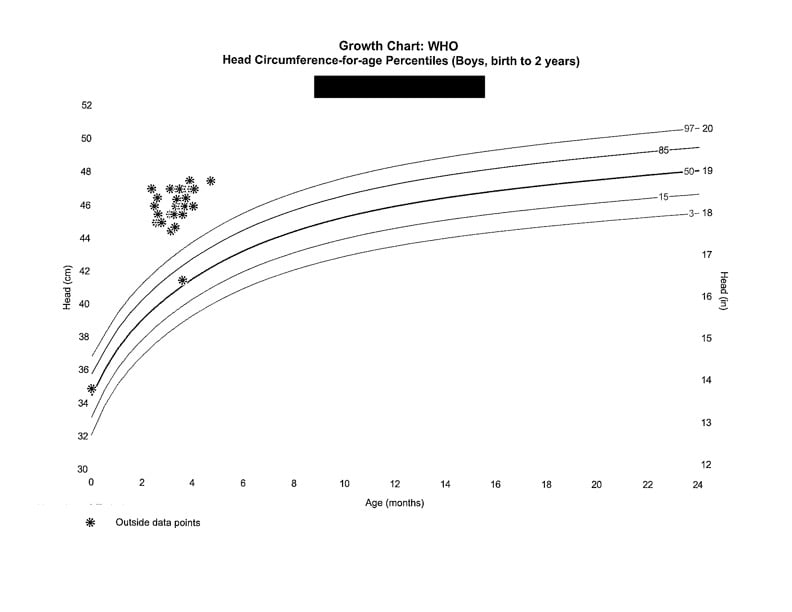
Figure 1
Laboratory evaluation was significant for a sodium of 128, potassium of 4.3, and creatinine 0.20. CBC was significant for a white blood cell count 19.0, hemoglobin 8.5, and platelets 1,086. Computed tomography of head without contrast demonstrated a large left-sided intracranial abscess with marked enlargement of the right lateral and third ventricles, concerning for obstructive hydrocephalus (Figure 2).
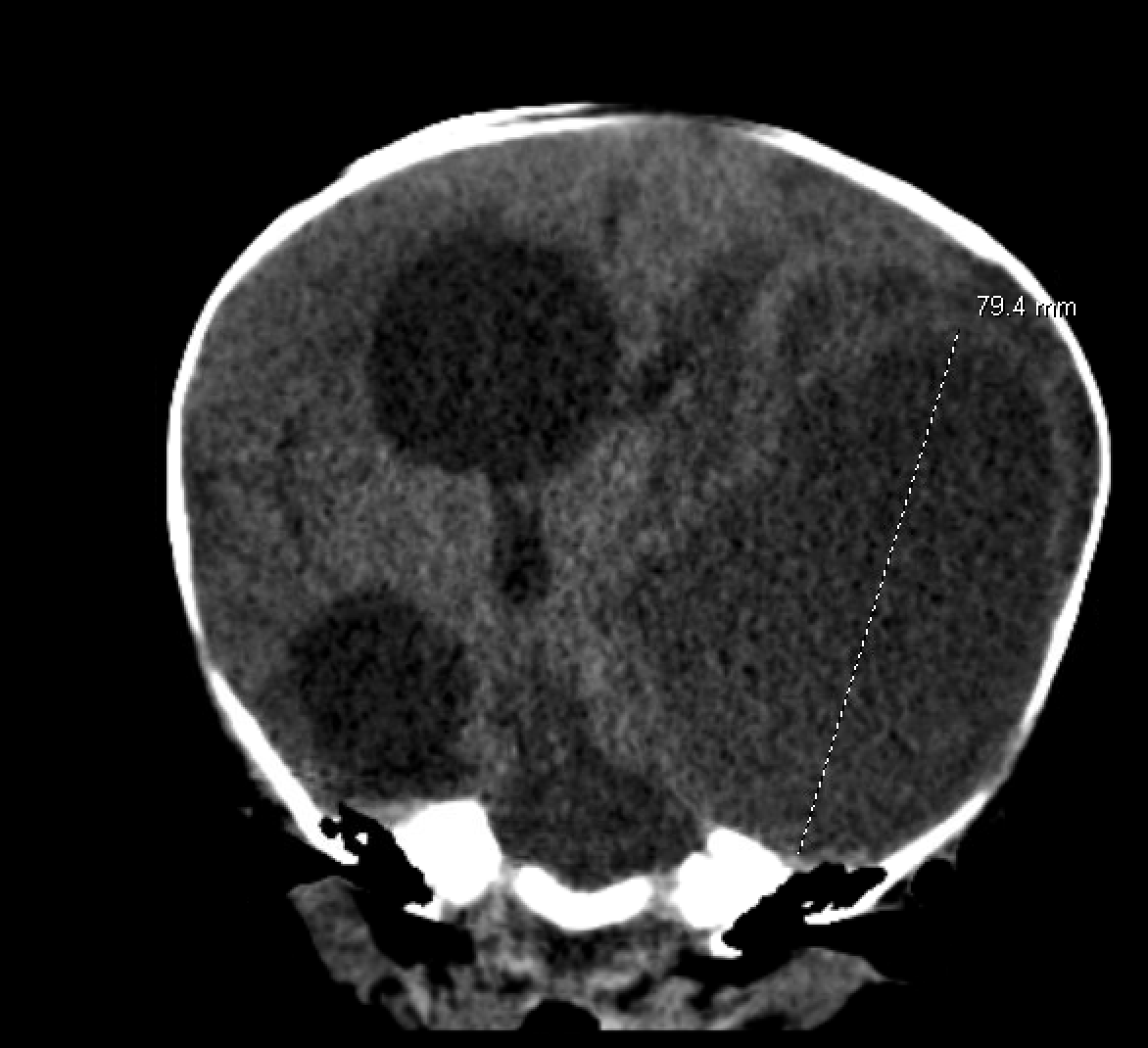
Figure 2
Neurosurgery was consulted, who recommended MRI and surgical management following advanced imaging. MRI revealed a large multiloculated left cerebral hemispheric abscess with marked mass effect including 1.5 cm of rightward midline shift, entrapment of the right lateral and third ventricles with associated transependymal edema, and left uncal herniation resulting in compression of the midbrain (Figure 3).

Figure 3
The patient was admitted to the pediatric ICU for close neurologic monitoring prior to neurosurgical intervention. Neurosurgery performed a craniotomy with washout of the abscess. On surgical inspection, frank purulent fluid was within the ventricles. Extensive washout was performed and an extraventricular drain was placed. Cultures were obtained from the intracranial abscess and ultimately grew Bacteroides fragilis. He was treated with vancomycin, cefepime, and metronidazole, which was eventually transitioned to vancomycin and meropenem. Several days later, a ventriculoperitoneal (VP) shunt was placed. After a 13-day hospitalization, he was discharged on a course of outpatient parenteral antibiotic therapy of meropenem and vancomycin. Upon review of subsequent outpatient pediatric visit notes, the patient was noted to be doing well overall with mild developmental delays.
Discussion
This is a unique case of a spontaneous intracranial abscess in an infant without significant past medical history. Brain abscesses are a rare pathology, caused by an intracranial collection of purulent fluid within the intraparenchymal space. Etiology of the abscess typically arises from direct local spread, such as sinusitis or acute otitis media or from hematogenous spread from other primary infection sites, most commonly pulmonary infections.2 Empiric broad spectrum antibiotic therapy is recommended and should be initiated in the emergency department. Ceftriaxone, metronidazole, and vancomycin are the preferred initial therapy regimen. Once culture results are available, the patient can be transitioned to a pathogen-specific regimen and will typically require a 4-6 week oral antibiotic course.3 Surgical management is often required; however, if the abscess is <2cm, there are multiple abscesses, there is no significant mass effect from the abscess, or the patient does not have significant neurologic deficits, antibiotic therapy alone may be sufficient.4
This is a unique case, as it appears that the patient had no preceding infection such as otitis media, upper respiratory infection, or ocular infection. In addition, the patient had no systemic signs of infection, including fever, and his blood cultures were negative. He underwent an extensive immunologic evaluation during his hospitalization and he was found to have no significant immunosuppressive pathology. It is unclear why this patient developed such an atypical pathology with an unusual pathogen.
While this case demonstrates a unique pathology of a spontaneous intracranial abscess in an infant, it highlights the importance of the use of head circumference measurements in the emergency department. Changes in head circumference can be critical for the early detection of other intracranial pathologies such as intracranial malignancies, hydrocephalus, meningitis, or benign enlargement of the subarachnoid spaces in infancy (BESSI). This measurement is a routine assessment in the outpatient pediatric setting and is typically obtained alongside weight and height. However, this is not commonly done in the emergency department, which could lead to missing subtle changes that could be the result of severe intracranial pathology. Trends in head circumference are particularly important as a rapid increase in head circumference is more indicative of intracranial pathology, as demonstrated in this case.
Conclusion
Head circumference measurements are a helpful objective tool that can aid in the diagnosis of many intracranial pathologies, as described in the case above, with a rare case of intracranial abscess. Obtaining head circumference measurements in the pediatric emergency department and comparing them to priors can be useful to aid in diagnosing intracranial pathologies early that may otherwise go unnoticed, particularly in an undifferentiated fussy infant.
References
- Muzumdar D, Jhawar S, Goel A. Brain abscess: An overview. International Journal of Surgery. November 16, 2010. Accessed June 24, 2025.
- Hall WA, Mesfin F. Brain abscess. StatPearls. September 21, 2024. Accessed June 24, 2025.
- Mameli, C., Genoni, T., Madia, C. et al. Brain abscess in pediatric age: a review. Child’s Nerv Syst 35, 1117–1128 (2019).
- Sheppard JP, Nguyen T, Alkhalid Y, Beckett JS, Salamon N, Yang I. Risk of Brain Tumor Induction from Pediatric Head CT Procedures: A Systematic Literature Review. Brain Tumor Res Treat. 2018 Apr;6(1):1-7.