The treatment of choice for a pneumothorax is a chest tube, and when the small pig-tail catheter doesn’t do the job, the answer is to replace it with a larger bore – right? Not so fast.
Case
A 39-year-old male presented to the emergency department with the chief complaint of difficulty breathing after being punched in the chest 3 days prior. On arrival, a chest x-ray (CXR) was obtained (Figure 1), revealing a left pneumothorax and associated lateral 6th rib fracture.
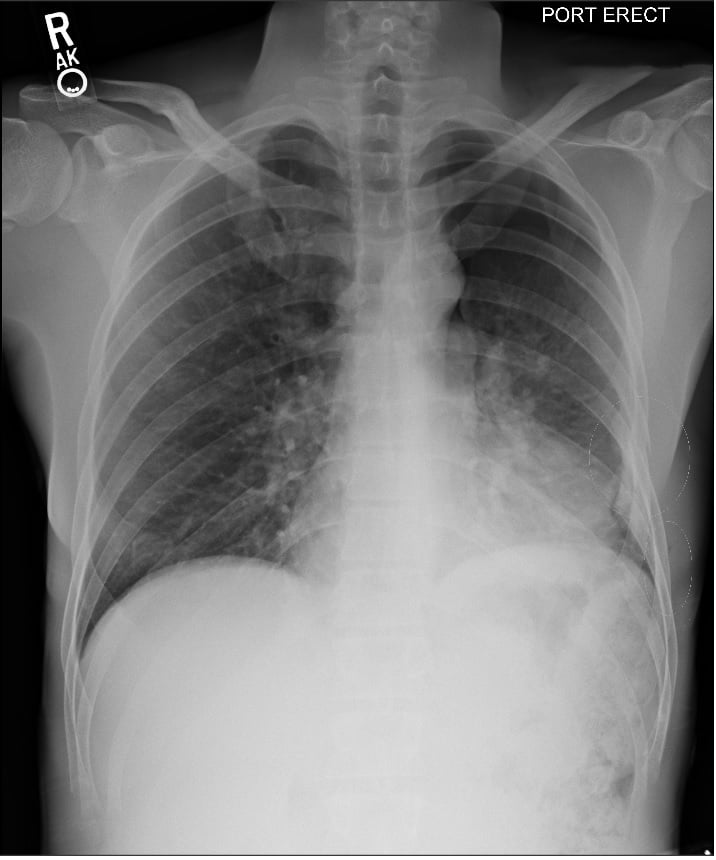
FIGURE 1. Initial CXR at 18:32 showing a large pneumothorax in the left upper lobe along with a fracture of the lateral aspect of the sixth rib. (white circular markings)
A small-bore chest tube (pig-tail catheter) was placed. After placement, the patient continued to complain of shortness of breath, developing new hypoxemia. Despite the confirmation of the pig-tail catheter on CXR (Figure 2), a large-bore chest tube was placed instead without any clinical improvement.
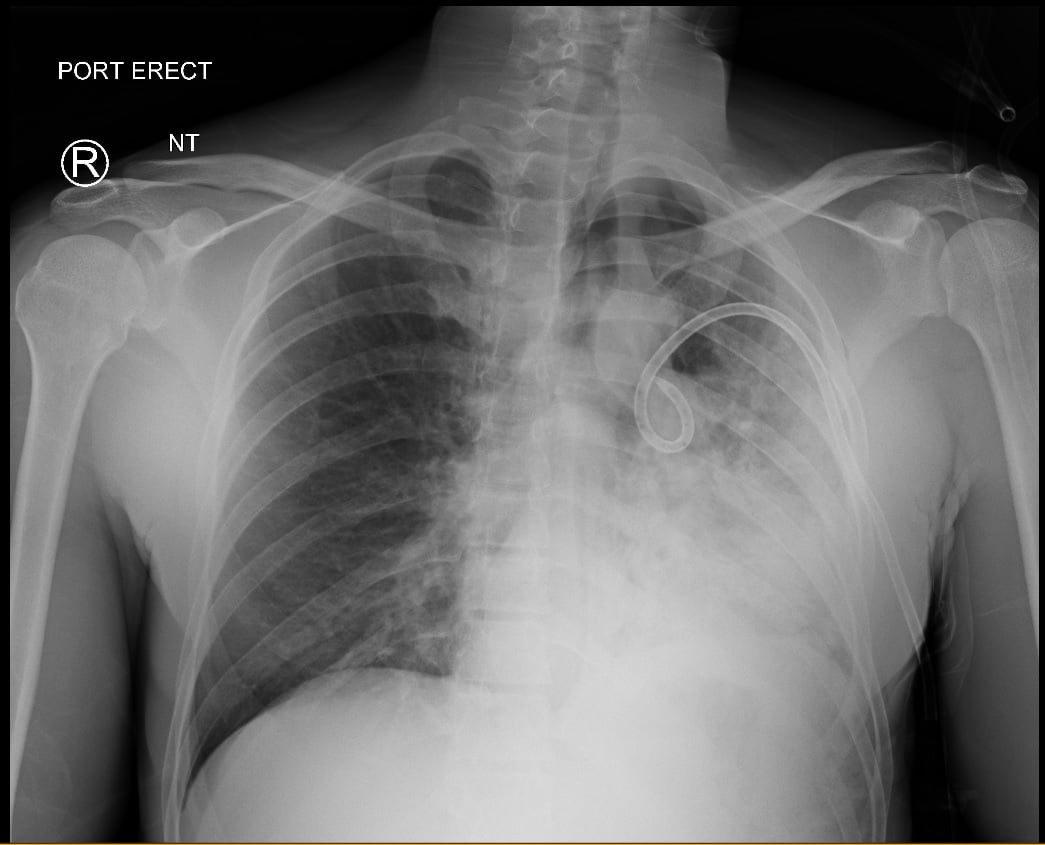
FIGURE 2. Second CXR at 20:01 confirming placement of a small caliber thoracostomy tube and new consolidation in the left lower lung.
The patient demonstrated persistent hypoxia and worsening tachypnea subsequently requiring intubation for hypoxic respiratory failure. Repeat CXR to confirm endotracheal tube placement showed worsening fluid accumulation in the affected lung (Figure 3).

FIGURE 3. Third CXR at 22:05 displaying an appropriately placed endotracheal tube, a large bore thoracostomy tube replacing the small caliber thoracostomy tube, and worsened opacification of the left thorax
So, what happened? More important: How do we fix it?
The treatment of choice for a pneumothorax is a chest tube, and when the small pig-tail catheter doesn’t do the job, the answer is to replace it with a larger bore – right?
Diagnosis
The exact mechanism of REPE is not clear. The current theory is that lung expansion leads to increased vascular permeability. Rapid inflow of blood to atelectatic lung segments results in an increase in both pulmonary capillary and hydrostatic pressures.1,2 The increased flow and permeability in the setting of alveolar injury contribute to the transudation of inflammatory mediators into the lung.3 Inflammatory molecules such as nitric oxide and free radicals alter capillary permeability leading to pulmonary edema and the clinical symptoms of hypoxia and tachypnea as seen in the aforementioned patient.4-6
The amount of time the lung remains collapsed is a major contributing factor of REPE. The timeline varies, with several cases reporting REPE’s onset from hours after lung collapse to between 3 and 7 days.2-4, 6- 8 REPE is often diagnosed on CXR; however, clinical symptoms of tachypnea and dyspnea generally develop within less than an hour of chest tube thoracostomy.9 In the aforementioned case, chest trauma in the preceding 3 days as well as the persistence of symptoms after appropriate chest tube placement offer strong supporting evidence for REPE.
How is REPE treated? The mainstay therapy for mild cases is well-described in the literature and consists of supplemental oxygen and cautious diuresis. The mechanism of REPE is different from that of cardiogenic edema.3, 7,10 Unlike cardiogenic edema, the rapid onset of fluid in REPE results from increased hydrostatic pressure because of alveolar and capillary inflammation.3 Therefore, treatment goals should focus on returning the vascular permeability, altered by this inflammation, to its original balanced state. Anti-inflammatory medications have proven to be beneficial once the diagnosis is suspected, Trachiotis et al. optimized on the cytoprotective actions of misoprostol and ibuprofen with resolution of REPE within 24-72 hours.10
For severe cases, where intubation and mechanical ventilation is necessary, there are several options described:
- Position the patient in the lateral decubitus position with the affected side up to reduce intrapulmonary shunting secondary to edema.1,3,10
- Apply more positive end-expiratory pressure (PEEP) and decrease tidal volumes to prevent further alveolar injury and transudation.
- Use of asynchronous differential lung ventilation. Described by Cho et al in a case report, this treatment method involves the use of a double lumen endobronchial tube and two ventilators each connected to a lung. The second ventilator utilizes a PEEP of 5 cm H2O for the REPE lung in order to assist its poor compliance and resolve the lung’s overall state of hyperperfusion. Improvement in the patient’s vital signs and arterial blood gas analysis were appreciated within 3 hours of asynchronous ventilation. This patient continued to improve over the next 6 days ultimately leading to extubation and eventually hospital discharge.
While the recognition and treatment of a pneumothorax in the ED is vital and can be gratifying, it is equally important to beware of the complications of our interventions. It is vital that emergency physicians performing chest tube placement understand the pathophysiology of REPE and its treatment. Awareness of its occurrence in high-risk patients may allow for more immediate recognition of its presence and earlier intervention, potentially preventing deterioration and respiratory failure. Proper knowledge of ventilator management and the potential use of novel techniques such as asynchronous differential lung ventilation may improve treatment for this high-severity condition.
References
1. Mahfood S, Hix WR, Aaron BL, Blaes P, Watson DC. Reexpansion pulmonary edema. Ann Thorac Surg. 1988;45(3):340-345.
2. Mahajan VK, Simon M, Huber GL. Reexpansion pulmonary edema. Chest. 1979;75(2):192-194.
3. Genofre EH, Vargas FS, Teixeira LR, Vaz MA, Marchi E. Reexpansion pulmonary edema. J Pneumol. 2003;29(2).
4. Kernodle DS, DiRaimondo CR, Fulkerson WJ. Reexpansion pulmonary edema after pneumothorax. South Med J. 1984;77(3):318-322.
5. Shanahan MX, Monk I, Richards HJ. Unilateral pulmonary oedema following re-expansion of pneumothorax. Anaesth Intensive Care. 1975; 3:19-30.
6. Sohara Y. Reexpansion pulmonary edema. Ann Thorac Cardiovasc Surg. 2008;14:205-209.
7. Rozenman J, Yellin A, Simansky DA, Shiner RJ. Re-expansion pulmonary oedema following spontaneous pneumothorax. Respir Med. 1996;90:235-238.
8. Humphreys RL, Berne AS. Rapid re-expansion of pneumothorax. Radiology. 1970;96: 509-512.
9. Matsuura Y, Nominura T, Murakami H, Matsushima T, Kalehashi M, Kajihara H. Clinical analysis of re-expansion pulmonary edema. Chest. 1991;100(6):1562-1566.
10. Trachiotis GD, Vricella LA, Aaron BL, Hix WR. Reexpansion pulmonary edema. Ann Thorac Surg. 1997;63(4):1205-1206.
11. Cho SR, Lee JS, Kim MS. New Treatment Method for Reexpansion Pulmonary Edema: Differential Lung Ventilation. Ann Thorac Surg. 2005;80(5):1933-1934.



