Signs of posterior sternoclavicular joint dislocations can be subtle, but this condition is a true orthopedic emergency. Are you prepared to perform a reduction in the ED if necessary?
An 11-year-old male presents to the ED with inability to move the right upper extremity because of pain. He was playing pick-up football at school about an hour prior to arrival. He tackled his opponent, and they both fell to the ground. The patient landed onto the point of his right shoulder with his opponent landing directly on top of him. Immediately, he noted significant pain in the right upper chest and shoulder that was exacerbated by any right upper extremity movement. His mother brought him to the ED for further evaluation and management.
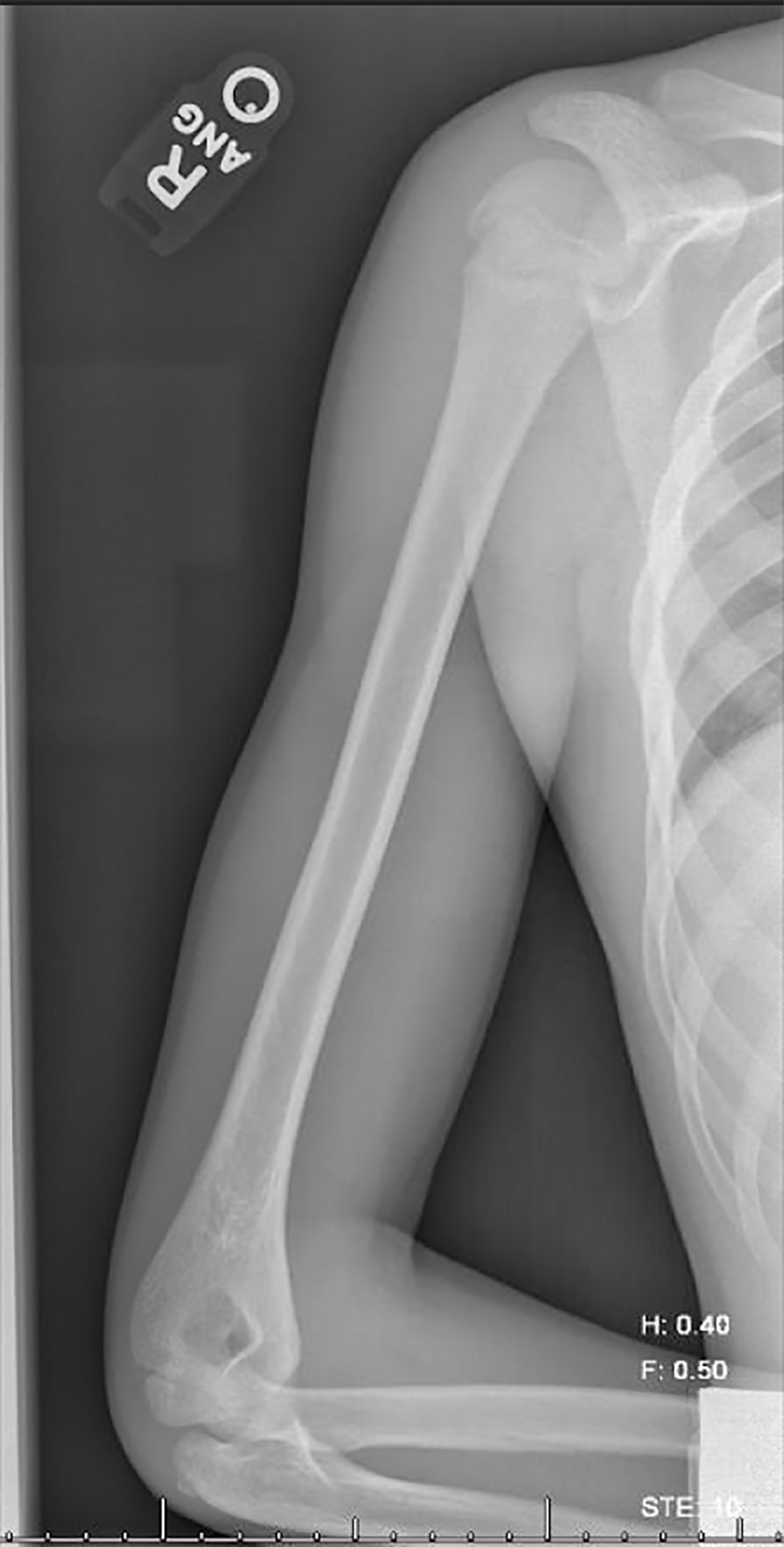
On exam, his right upper extremity was maintained in flexion at the elbow and internally rotated, his left hand holding the right elbow in a stable position. He was noted to be in severe pain. He was neurovascularly intact with no dysphagia or dyspnea. His lungs were clear to auscultation. Plain films of the chest, shoulder, clavicle, and humerus were obtained and showed no occult injury. (Figure 1, 2, 3, 4)
The patient was still in severe pain despite analgesia, so the decision was made to obtain a CT of the chest (Figure 5). The CT demonstrated a right posterior sternoclavicular (SC) joint dislocation. The clavicle was noted to be displaced posteriorly into the mediastinum. There was no evidence of vascular injury. A possible small cortical fragment avulsion of the anterior aspect of the proximal right clavicle was noted.




Clinical Picture
On inspection, posterior SC dislocations are usually more subtle than anterior SC dislocations. An anterior dislocation will most likely present with a bulge at the site, while a posterior dislocation will often be a minor depression. If the time between injury and presentation to the ED is delayed, more obvious swelling overlying the joint might be appreciated. A posterior SC dislocation is typically caused by indirect lateral shoulder compression instead of direct impact at the joint. Our patient’s injury was caused by an indirect lateral compression at the shoulder.
Most patients will not want to move their upper extremity because of pain at the SC joint.1 They must be evaluated for severe life-threatening findings such as aerodigestive and neurovascular compromise. This manifests clinically as stridor, dysphagia, shortness of breath, sensation loss, and pulse deficits.
The SC joint is the only true articular joint between the arm and the axial skeleton.2 It participates in all movements of the upper extremity. So, any movement at the shoulder will elicit pain when this joint is disrupted. In addition, patients often do not tolerate lying supine because of pain.
Because of the vital structures that lie posterior to the medial clavicle (the innominate artery, innominate vein, brachial plexus, trachea, superior lung, esophagus, and thoracic duct), a posterior sternoclavicular joint dislocation makes this a true orthopedic emergency.
Imaging Difficulties
This case highlights the difficulty of seeing a posterior sternoclavicular dislocation on plain films. Radiographs have low sensitivity, but are important for ruling out a pneumothorax, pneumo.mediastinum, and hemopneumothorax. Sometimes, imaging can demonstrate the asymmetric and inferiorly displaced medial clavicle. However, as in our initial CXR (Figure 1), the displacement on plain films is not apparent. The repeat CXR impression was read as “In retrospect, there is a slight offset of the medial clavicles at the sternoclavicular joint, which was subsequently proven to represent a right posterior sternoclavicular dislocation by CT.” Again, this is common not to see a dislocation on an AP or PA view.
If CT or MRI are not readily available, then obtain a serendipity view. This is a plain film of the chest angled at 40 degrees cephalad. The preferred imaging would be an MRI/MRA or CT/CTA chest, depending on what is available at your site.3
Reduction
Consult Orthopedics immediately. If they are unavailable at your facility and the patient starts having aerodigestive or neurovascular compromise, then reduction should be attempted immediately in the ED.
First, obtain consent for the sedation and reduction, then sedate the patient.
Place the patient in a supine position with a rolled towel positioned between the scapula and the table. Have the affected arm to the edge of the bed, abducted, use traction and countertraction. This is usually about 80% successful.2 If this doesn’t work and you have Orthopedics available, then use sterile towel clips and apply percutaneously around the clavicle. Continue with anterior traction of the clavicle with countertraction of the upper extremity. Some sources recommend admission for observation due to potential injury to important structures if it dislocates again.4 Others recommend applying a post reduction figure-eight sling and follow up with Orthopedics in 4–6 weeks to allow for ligamentous healing.2
Another reduction technique in the literature is the Buckerfield and Castle. While shoulders are pushed posteriorly by an assistant, the ipsilateral arm is adducted against the torso and caudal traction is applied.
Important Facts
The superior mediastinum runs just posterior to the medial portion of the clavicles. Sternoclavicular dislocations account for less than 1% of all dislocation injuries. Although the diagnosis is rare, if you have a patient presenting with a posterior sternoclavicular dislocation, the patient will have a 30% chance of developing life-threatening complications.2
The SC joint has the least amount of bony stability of any major joint in the body, as less than half of the medial end of the clavicle articulates with the upper sternum. The medial clavicular epiphysis is the last epiphysis of the body to appear radiographically at 18 years old, and the last to close at the age of 22-25 years old.5 This means younger patients are less likely to dislocate and more likely to fracture.
Pearls
Interestingly, on this patient there was a small cortical fracture fragment that had avulsed from the anterior aspect of the proximal right clavicle. The cortical fragment was likely present because the epiphyseal plate had not yet fused because the patient was 11 years old. As stated previously, the physis of the medial clavicle remains open until 22–25 years of age.5 One would think the patient would have a more pronounced fracture and not a dislocation due to the non-closure of the epiphysis.6 Thus, even in this age group (<18 years old) consideration of posterior sternoclavicular dislocation is critical for the differential diagnosis.
Case Conclusion
Our patient was taken to the operating room with Orthopedics and Cardiothoracic Surgery on standby. The patient underwent a successful reduction in the OR and has had no complications to date.
Take-home Point
If there is suspicion for posterior sternoclavicular joint dislocation, then obtain CT or MRI if available. If not, get a serendipity view. If Orthopedics is not available, consider options of reduction and attempt the closed reduction technique. If successful, place the patient in a figure-eight sling and have them follow up with Ortho in the next 4–6 weeks. If not, transfer the patient to a hospital with Orthopedics and Cardiothoracic Surgery consultants.
References
1. Astin M. Sternoclavicular Joint Dislocations: Diagnosis and Treatment. ALiEM. 2014.
2. Roepke C, Kleiner M, Jhun P, Bright A, Herbert M. Chest Pain Bounce-Back: Posterior Sternoclavicular Dislocation. Ann Emerg Med. 2015;66(5):559-561.
3. Dr. David Geier Enterprises. Sternoclavicular Dislocation. 2018.
4. Ostermayer D, Snyder J, Swartz J, Donaldson R, Young N. Sternoclavicular Dislocation. WikEM.
5. Bjorensen LP, Ebinger A. Shoulder and Humerus Injuries. In: Tintinalli JE, Stapczynski S, Ma OJ, et al, ed. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. New York, NY: McGraw Hill Education;2016.
6. Cadogan M. Sternoclavicular Joint Dislocation. Life in the Fast Lane. 2017.



