Background
Splenic rupture refers to the disruption of the splenic capsule or tearing apart of the spleen, a vital organ responsible for filtering blood and fighting infections. This condition is considered a medical emergency, as it can cause significant and potentially life-threatening internal bleeding.1
Splenic rupture occurs primarily as a result of blunt trauma to the abdomen, such as from a car accident or a fall. Certain medical conditions that affect the spleen — including mononucleosis (EBV), leukemia, or lymphoma — are less common but still important causes of splenic rupture.1
Case Report
A 71-year-old male with a history of hypertension and hyperlipidemia was brought to the emergency department by his wife after experiencing a mechanical fall at home. The patient had been recovering from a recent viral illness and had been experiencing balance issues. He had been taking apixaban for the past year due to an episode of atrial fibrillation in addition to his antihypertensive medication. His Glasgow Coma Scale was 15 at the time of arrival at the ED. When questioned, the patient denied losing consciousness during the fall.
The physical exam revealed an elderly gentleman in acute distress with a 4-cm laceration noted to the left temporal scalp. No depressed skull fracture was noted. The exam was otherwise within normal limits. The patient’s vitals were HR 74 bpm, RR 20/min, BP 94/62 mmHg, and O2 sat 95%. An ECG was normal sinus rhythm without ectopic or ischemic changes, and a viral panel was positive for influenza A. A complete blood count (CBC) revealed a low hemoglobin of 10.7 g/dl and hematocrit of 32.8%. A CT of the head without contrast was performed to rule out cerebral hemorrhage, and there was no acute intracranial abnormality noted. The patient received staples for his scalp laceration and was discharged from the ED.
Nine hours later, however, the patient returned to the ED complaining of dizziness and lightheadedness that intensified with any change in body position. The only abnormality on the patient’s physical exam at this time was the pallor of his skin. Although he had a regular rate and rhythm, he had a worrisome blood pressure of 69/48 mmHg. He was given a normal saline fluid bolus, and a CBC, complete metabolic panel (CMP), and troponin were ordered. Two serial ECGs both showed normal sinus rhythm with no immediate ST-T changes, and the troponin levels came back within normal limits. However, the CMP results showed that the patient’s BUN and Cr levels were elevated. On the review of the repeat CBC, the patient’s hemoglobin levels had plummeted to 6.0 g/dl and hematocrit to 19.2%.
The emergency physician immediately ordered a CT scan of the chest and abdomen with contrast to pinpoint the source of the bleeding. Soon thereafter, the physician received a call from the radiologist, who informed him that the patient had a ruptured spleen. The CT scan of the abdomen revealed a large subcapsular hematoma compressing the spleen, with mild-to-moderate serosanguineous ascites. Subcapsular venous extravasation was noted under the lateral splenic capsule. To stabilize the patient, the team sent a type and crossmatch and administered 4 units of blood before transferring him via medevac for immediate surgical intervention.

Figure 1: CT abdomen with contrast revealing a large subcapsular hematoma compressing the spleen, with mild to moderate serosanguineous ascites. Subcapsular venous extravasation noted under the lateral splenic capsule.

Figure 2: CT abdomen with contrast revealing a large subcapsular hematoma compressing the spleen, with mild to moderate serosanguineous ascites. Subcapsular venous extravasation noted under the lateral splenic capsule.

Figure 3: Left upper quadrant (splenorenal) view. (a) Transducer placement at the left upper quadrant (LUQ). (b) Illustration of transducer placement and relevant anatomy. (c) Normal ultrasound image of the splenorenal space or left upper quadrant. (d) Illustration of important structures visualized in the ultrasound image including the kidney, diaphragm, and spleen. Artwork (a) created by Emily Evans © Cambridge University Press. Illustration (d) by Laura Berg, MD.10 Images used with permission. Disclaimer: The images provided in Figure 3 are not the FAST images from our patient, but rather a demonstration of a negative FAST in the LUQ.
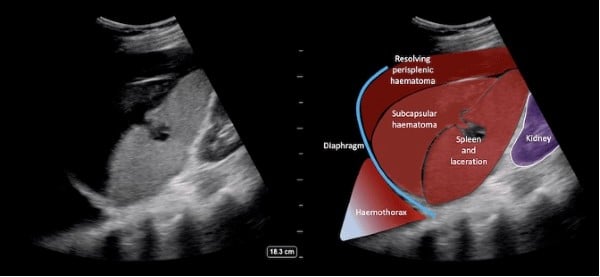
Figure 4: FAST left upper quadrant view showing that there is heterogeneous predominantly hyperechoic perisplenic hematoma as well as subcapsular hematoma. The echogenic area in the mid-portion of the spleen disturbing the usual homogeneous echotexture suggests a laceration.11 Image used with permission. Disclaimer: The FAST images provided are not the FAST images from our patient, but rather a positive FAST in the LUQ.
Case Discussion
Splenic rupture is generally categorized into traumatic and atraumatic causes. Traumatic splenic rupture typically results from blunt abdominal trauma, including compressive forces against the abdomen or shearing forces created by sudden deceleration.2 The most susceptible patients are older adults, alcoholic patients, and in the case of motor vehicle accidents, those wearing safety belts without shoulder attachments.3 Lacerations of the spleen can occur from fractured ribs or pelvic bones, and a history of trauma to the left upper quadrant, left rib cage, or left flank should increase suspicion of splenic injury.4 Patients with traumatic splenic rupture may present with left upper abdominal, left chest wall, or left shoulder pain from diaphragm irritation, also known as Kehr’s sign.3,5 Fox’s sign may be present as bruising over the outer aspect of the thigh, delineating that there is active retroperitoneal bleeding.6 Other physical manifestations include left upper quadrant or generalized abdominal tenderness, abdominal wall contusion or hematoma (e.g., seatbelt sign), and left lower chest wall tenderness, contusion, or instability due to rib fractures.3
Atraumatic splenic rupture (ASR) is less common but can occur in a wide age range, from teenagers to the elderly. The majority of cases are “pathologic” ASRs, meaning they develop in a diseased spleen due to infection, coagulopathy, or neoplasm.7 In some cases, ASR represents the initial manifestation of an underlying disease. Alternatively, “idiopathic” ASR can occur in a normal-appearing spleen without predisposing factors. Anticoagulation is a common cause of idiopathic ASR, accounting for up to 9% of cases.7 Patients with ASR may present with variable degrees of upper or left-sided abdominal pain, tachycardia, and hypotension, followed by malaise, vomiting, generalized abdominal tenderness, peritonitis, and progressive hemodynamic shock.8
In the case of this patient, there were many variables that likely contributed to his splenic rupture: his fall, anticoagulation therapy, and a recent history of influenza A. Key details surrounding the nature and mechanism of this patient’s fall — such as his position at the time of the incident, the height of the fall, and what triggered the fall — remain limited. On his initial presentation, the patient’s hypotension and history of a recent fall did raise the suspicion for another injury apart from his scalp laceration; however, he denied any abdominal pain on physical exam. His past medical history of atrial fibrillation and anticoagulation with apixaban increased his risk for spontaneous bleeding and, theoretically, for atraumatic splenic rupture. Similarly, his recent viral illness also could have played a role in causing ASR.9
While the exact cause of this patient’s splenic rupture was most likely the combination of his anticoagulation therapy and his fall, this case is presented as a noteworthy example of how splenic rupture can occur in the absence of overt physical exam findings. On physical exam, the patient had negative Kehr’s sign, negative Fox’s sign, and no abdominal pain or rebound tenderness to palpation. This demonstrates that splenic rupture cannot be excluded from the differential due to an unremarkable physical examination in the appropriate clinical scenario. A Focused Assessment with Sonography in Trauma (FAST) was not deemed to be warranted on his initial presentation due to the absence of any positive physical exam findings; however, perhaps his hypotension should have prompted further pursuit of an explanation apart from the fact that he took his blood pressure medications earlier that morning. Nonetheless, the FAST exam is a critical diagnostic tool that should always be considered in a patient presenting with hypotension with or without a low hemoglobin.
Case Conclusion
In summary, splenic rupture is generally classified into two categories: traumatic and atraumatic. The former is typically the result of blunt abdominal trauma, while the latter can occur due to a variety of pathologic causes, such as infection, malignancy, and systemic anticoagulation. This patient’s case of splenic rupture was interesting as he not only had a history of trauma and anticoagulation use, but he also had a recent history of viral illness. This case serves as a sobering reminder that even in the absence of any remarkable findings on a physical abdominal exam, it is essential for emergency physicians to keep the possibility of splenic rupture in mind and consider performing a FAST in the setting of unexplained abnormal vital signs.
References
- Waseem M, Bjerke S. Splenic Injury. PubMed. Published 2020. Accessed April 19, 2023.https://www.ncbi.nlm.nih.gov/books/NBK441993
- Davis JJ, Cohn I, Nance FC. Diagnosis and management of blunt abdominal trauma. Annals of Surgery. 1976;183(6):672-678. doi:https://doi.org/10.1097/00000658-197606000-00009
- Diercks DB, Clarke SO. Initial evaluation and management of blunt abdominal trauma in adults. Uptodate.com. Published 2020. Accessed April 19, 2023. https://www.uptodate.com/contents/initial-evaluation-and-management-of-blunt-abdominal-trauma-in-adults
- Maung A, Kaplan L. UpToDate. www.uptodate.com. Accessed April 19, 2023. https://www.uptodate.com/contents/management-of-splenic-injury-in-the-adult-trauma-patient?search=spleen%20rupture&source=search_result&selectedTitle=1~60&usage_type=default&display_rank=1
- Marx JA, Isenhour JL. Initial Evaluation and Management of Blunt Abdominal Trauma in Adults. Uptodate.com. Published 2006. Accessed April 19, 2023. https://www.uptodate.com/contents/initial-evaluation-and-management-of-blunt-abdominal-trauma-in-adults
- Fox’s sign. DBpedia. Published 2023. Accessed April 19, 2023. https://dbpedia.org/page/Fox%27s_sign
- Bona R. Splenomegaly and Other Splenic Disorders in Adults. www.uptodate.com. Published February 10, 2023. Accessed April 19, 2023. https://www.uptodate.com/contents/splenomegaly-and-other-splenic-disorders-in-adults?search=atraumatic%20splenic%20rupture%20etiology&source=search_result&selectedTitle=1~149&usage_type=default&display_rank=1#
- Tonolini M, Ierardi AM, Carrafiello G. Atraumatic splenic rupture, an underrated cause of acute abdomen. Insights into Imaging. 2016;7(4):641-646. doi:https://doi.org/10.1007/s13244-016-0500-y
- Deol D, Wu H, Lasso-Pirot A, Robinett KS, Diaz-Abad M. Atraumatic Splenic Rupture Associated with Influenza A (H1N1) Pneumonia: Case Report and Review of the Literature. Case Reports in Medicine. 2021;2021:e6516064. doi:https://doi.org/10.1155/2021/6516064
- Rippey J. "Ultrasound Case 104," In: LITFL - Life in the FastLane, Accessed on May 4, 2023, https://litfl.com/ultrasound-case-104/.
- Themes U. F. O. “The Extended Focused Assessment with Sonography for Trauma (E-FAST).” Anesthesia Key, 17 Feb. 2017, aneskey.com/the-extended-focused-assessment-with-sonography-for-trauma-e-fast/. Accessed 4 May 2023.