In the emergency department, high fever and altered mental status in elderly patients often suggest central nervous system infection or sepsis. Nevertheless, without early neuroimaging to rule out intracranial structural lesions, critical conditions such as intraventricular hemorrhage may be missed. This case involved a sudden fatal outcome in the emergency room despite aggressive intervention, highlighting the vital importance of early recognition and management.
Case presentation
An 88-year-old female with an unclear medical history was brought to the emergency department by her family due to high-grade fever (40°C), altered mental status, and unresponsiveness to verbal stimuli. On initial assessment, her Glasgow Coma Scale (GCS) score was 8, Auscultation revealed bilateral rales. The patient exhibited gasping respirations with an SpO₂ of 86% that was unresponsive to supplemental oxygen via face mask, tachycardia (118 bpm), and blood pressure of 155/95 mmHg. Due to the high risk of progressive respiratory failure and deep coma, she was intubated emergently in the emergency room.
Chest X-ray revealed diffuse bilateral pulmonary infiltrates, suspicious for pulmonary edema or pneumonia. Arterial blood gas analysis showed mild metabolic acidosis (pH 7.28, HCO₃⁻ 15 mmol/L, lactate 3.8 mmol/L). The patient remained hemodynamically stable without the need for vasopressors. Given the undetermined cause of her altered consciousness, lumbar puncture was deferred due to relative contraindications, and an emergent non-contrast head CT was ordered.
While returning from the imaging suite, the patient suffered a sudden cardiac and respiratory arrest with absent carotid pulse. Advanced cardiac life support (ACLS) was initiated immediately, but resuscitation was unsuccessful after 30 minutes. The patient was pronounced dead in the emergency department.
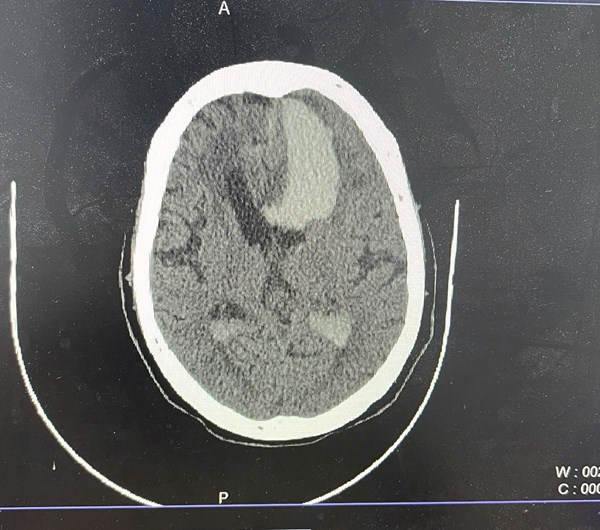
The head CT performed shortly before arrest revealed a large hemorrhage in the left basal ganglia, extending into the lateral and third ventricles, accompanied by diffuse cerebral edema and significant midline shift. These findings were consistent with severe intracranial pathology and an acute elevation in intracranial pressure, leading to brain herniation and loss of circulatory function.
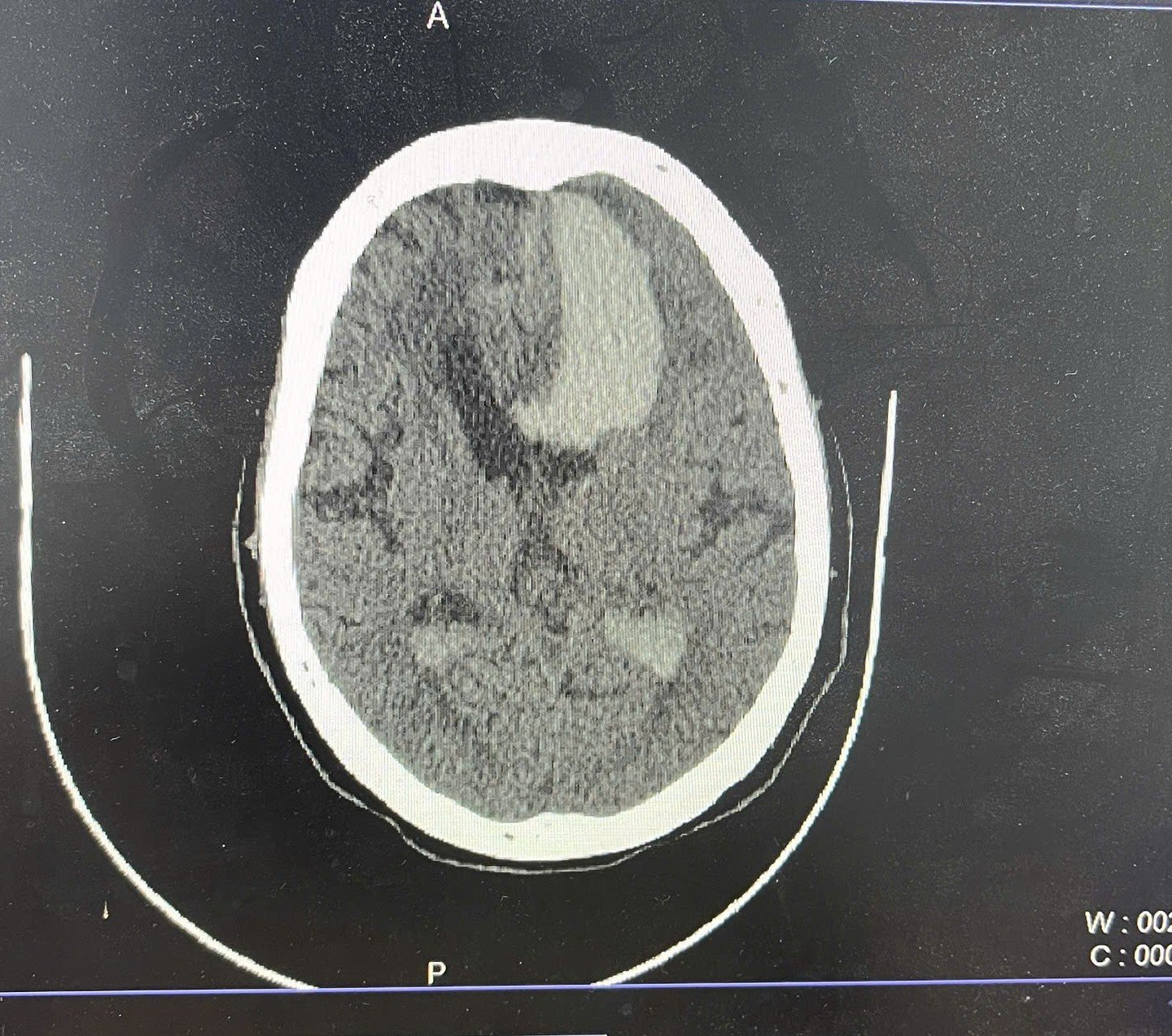
Figure 1. Non-contrast CT scan of the brain (axial view) demonstrates a large hyperdense hematoma in the left basal ganglia with extension into the left lateral ventricle. There is marked surrounding vasogenic edema, rightward midline shift, and compression of the contralateral lateral ventricle—findings consistent with mass effect and impending brain herniation.
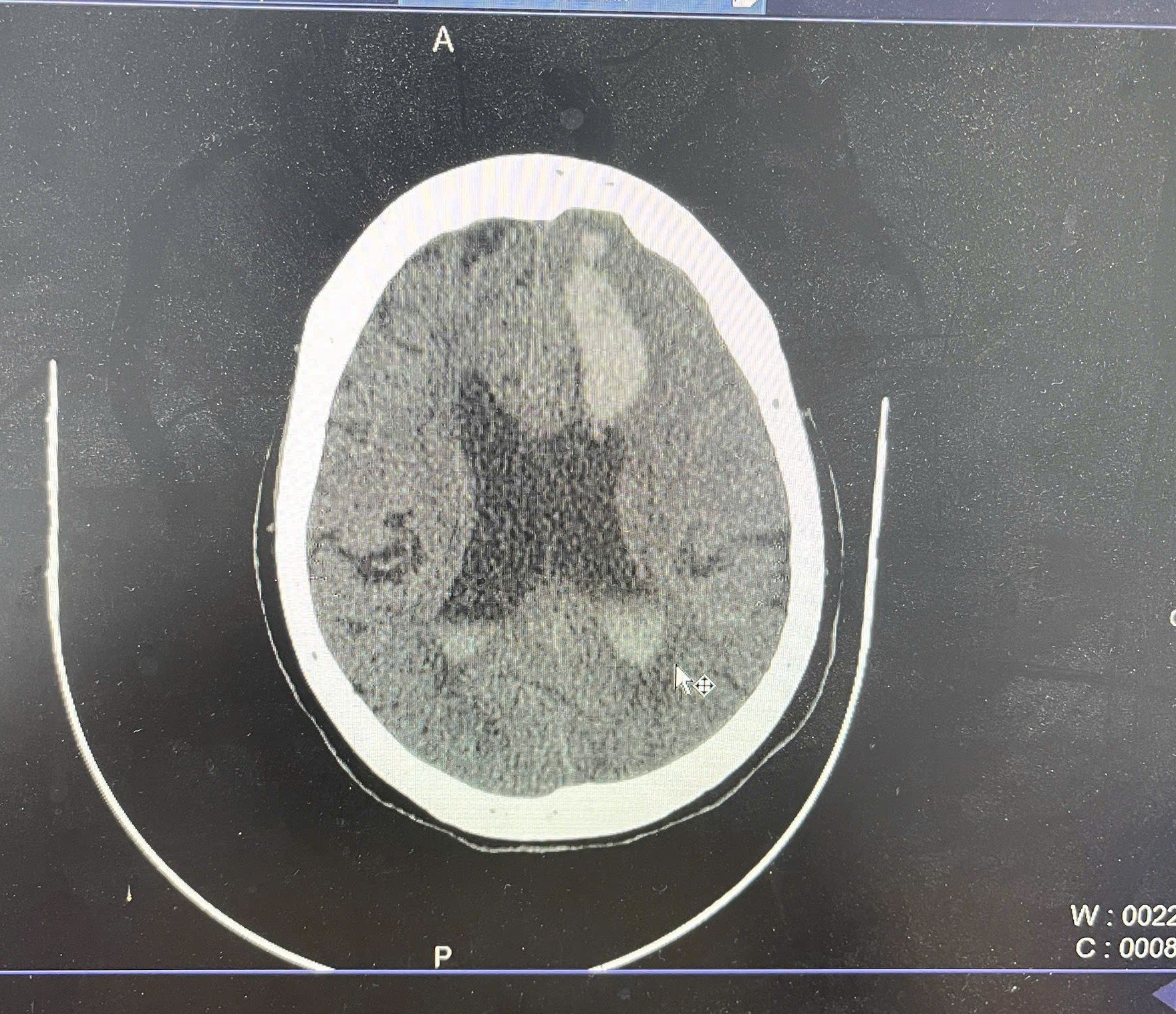
Figure 2. Non-contrast axial CT image at a higher level shows hyperdense hemorrhage in the left periventricular white matter and left lateral ventricle, consistent with intraparenchymal hemorrhage and intraventricular extension. There is surrounding hypodensity representing cerebral edema and rightward midline shift indicating mass effect.
Conclusion
An elderly female patient presented with high-grade fever, altered mental status, bilateral pulmonary crackles, and agonal breathing—a clinical scenario that may initially lead physicians to suspect respiratory infection or meningitis. However, an emergent non-contrast head CT subsequently revealed a large hemorrhage in the left basal ganglia extending into the lateral and third ventricles, accompanied by cerebral edema and midline shift. Although the CT scan was performed immediately after endotracheal intubation, the imaging had not yet been formally interpreted when the patient experienced sudden cardiac arrest during transport back to the emergency department.
Importantly, in this case, high fever may not necessarily indicate infection but could reflect central thermoregulatory dysfunction caused by hypothalamic irritation from the hematoma, or a systemic inflammatory response to the breakdown of red blood cells and hemoglobin in the brain parenchyma.1 The altered level of consciousness, which ranged from lethargy to deep coma, was likely a direct result of elevated intracranial pressure, diffuse cerebral edema, and reduced cerebral perfusion, particularly as intraventricular hemorrhage compressed the reticular activating system (RAS) and compromised cerebral perfusion pressure (CPP).2,3
Intracranial hypertension in basal ganglia hemorrhage typically progresses through three phases: an initial phase of local pressure from the hematoma, a secondary phase of mass effect from cerebral edema, and a decompensation phase, in which intracranial pressure (ICP) exceeds mean arterial pressure (MAP), leading to critically low CPP and global cerebral ischemia. At the same time, intraventricular blood provokes central inflammation, triggering the release of interleukin-6, TNF-alpha, and neurotoxins that damage the blood–brain barrier and promote cytotoxic edema.3
Furthermore, brainstem compression disrupts autonomic regulation of respiration and cardiovascular function, initially manifesting as transient Cushing's reflex (hypertension, bradycardia, irregular respiration) and ultimately progressing to irreversible cardiorespiratory arrest.4
Of note, agonal breathing, decreased SpO₂, and bilateral pulmonary crackles suggest neurogenic pulmonary edema—an often-overlooked complication. This condition may occur in 20–30% of patients with severe acute brain injury and is driven by a massive catecholamine surge that increases pulmonary capillary hydrostatic pressure and leads to alveolar fluid accumulation in the absence of true infection.5,6 Arterial blood gas analysis demonstrated metabolic acidosis and elevated lactate, indicating impaired tissue oxygenation secondary to global hypoperfusion.
The sudden cardiac arrest shortly after the CT scan was most likely due to acute brain herniation. The absence of hypotension or septic shock prior to the event renders extracerebral causes improbable. Earlier review of imaging and timely neurosurgical intervention—such as external ventricular drainage (EVD), osmotherapy with mannitol or hypertonic saline to control ICP, and preparation for transfer to a neurocritical care unit—might have provided a life-saving window.7,8
Poor prognostic indicators were present in this case, including intraventricular hemorrhage, diffuse cerebral edema, and midline shift >5 mm, all of which are associated with high 24-hour mortality despite intensive treatment.9
Differential Diagnosis in Elderly Patients with Fever and Altered Mental Status Includes:
- Acute meningitis or meningoencephalitis (bacterial or viral) is often suspected when fever, confusion, neck stiffness, seizures, and leukocytosis are present. However, neuroimaging is imperative before lumbar puncture to exclude mass effect.
- Sepsis with secondary neurological involvement: especially when there is evidence of pneumonia, urinary tract infection, or intra-abdominal infection, typically accompanied by hypotension and elevated lactate. In this case, the patient was not in shock, lowering this likelihood.
- Severe pneumonia with respiratory acidosis, agonal breathing, and hypoxia: may secondarily impair consciousness, particularly in the elderly. However, abnormal CT findings rule out this as a primary cause.
- Ischemic brainstem stroke or intracerebral hemorrhage is the most life-threatening cause and must be promptly excluded through early neuroimaging.
- Metabolic encephalopathy from hypoglycemia, hyponatremia, or uremia: also common in the elderly and should be investigated with urgent laboratory testing.
Clinicians are susceptible to anchoring bias when interpreting febrile presentations. The presence of fever, pulmonary crackles, and respiratory distress often results in a focus on pneumonia, meningitis, or sepsis, delaying consideration of central nervous system pathology. Without timely neuroimaging and appropriate contraindication-based decision-making regarding lumbar puncture, the risk of precipitating fatal brain herniation increases substantially.
In scenarios, emergency management should include: early ICP control with mannitol or hypertonic saline, prompt neurosurgical consultation for EVD placement, respiratory and circulatory support in a neuro-ICU setting, and evaluation for decompressive craniectomy if midline shift exceeds 5 mm. These interventions must be executed within the "golden window"—typically within 2 hours of symptom onset—to improve outcomes and reduce mortality.
From the perspective of an experienced neurocritical care physician, this case exemplifies a classic rapid-onset brain injury unfolding within the first hour. The clinical question is not “Should we order a CT scan?” but rather “Can we do it fast enough to save the patient?” This case also underscores the critical need for seamless coordination among emergency medicine, neurology, critical care, and radiology teams when managing patients with acute neurologic deterioration.
A brain hemorrhage doesn’t need hours to kill—it only needs minutes, a single delay, or one mistimed decision. In any patient with unexplained fever and altered mental status, head CT is not optional—it is a matter of life and death.
Clinical Implication
This case demonstrates the importance of maintaining a broad differential when evaluating febrile patients with altered mental status. Although respiratory signs are present, intracranial structural pathology must not be excluded without imaging. A non-contrast brain CT should be performed within 30 minutes in any patient presenting with fever, unexplained impaired consciousness. This process should occur in parallel with stabilization efforts, not afterward.
In many health care settings, early CT access may be limited by resource constraints or patient volume. This only reinforces the need to prioritize rapid pathways for acute neurologic emergencies. This case serves as a powerful lesson for emergency physicians, neurologists, and intensivists, especially when dealing with atypical yet high-risk presentations.
Learning Points
- Intracranial pathology should not be overlooked in elderly patients presenting with fever and altered mental status, even when accompanied by respiratory findings such as bilateral crackles or hypoxia.
- Non-contrast head CT is a life-saving investigation, not an optional test, in any patient with a Glasgow Coma Scale (GCS) <13 of unclear cause. It should be performed as early as possible, in parallel with airway and hemodynamic stabilization.
- Neurogenic pulmonary edema and agonal breathing may be early indicators of brainstem dysfunction or rising intracranial pressure and require urgent recognition and management.
- Brain herniation is a time-sensitive emergency that can lead to irreversible cardiopulmonary arrest within minutes to hours if not rapidly identified and treated.
- Cognitive bias is a dangerous pitfall, particularly in elderly patients with fever and decreased consciousness, and clinicians must maintain a broad differential and initiate early cross-disciplinary collaboration.
References
- Goyal K, Garg N, Bithal P. Central fever: a challenging clinical entity in neurocritical care. J Neurocritical Care. 2020 Jun 1;13(1):19–31.
- Davidson CL, Kumar A. Intracranial Hypertension. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 [cited 2025 Jun 15].
- Wan Y, Holste KG, Hua Y, Keep RF, Xi G. Brain edema formation and therapy after intracerebral hemorrhage. Neurobiol Dis. 2023 Jan 1;176:105948.
- Dinallo S, Waseem M. Cushing Reflex. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 [cited 2025 Jun 15].
- ACS [Internet]. [cited 2025 Jun 15]. A Systematic Review of Neurogenic Pulmonary Edema in Traumatic Brain Injury.
- Rajagopal R, Ganesh S, Vetrivel M. Neurogenic pulmonary edema in traumatic brain injury. Indian J Crit Care Med. 2017 May;21(5):329–31.
- Tenny S, Das JM, Thorell W. Intracranial Hemorrhage. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 [cited 2025 Jun 15].
- Ditkowsky J, Ullo M. Altered Mental Status: Geriatric Edition | Relias Media [Internet]. [cited 2025 Jun 15].
- Hemphill JC, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage. Stroke. 2015 Jul;46(7):2032–60.