Esophageal food impaction is a common emergency, typically linked to intrinsic esophageal pathologies. While most cases stem from issues like Schatzki's ring or strictures, rare instances can arise from extrinsic structural compression. This report details an unusual case caused by such an extrinsic factor and the utility of CT imaging in guiding the diagnosis.
Case Report
A 62-year-old woman presented with a 12-hour history of food impaction, a recurring issue that had previously resolved spontaneously but failed to do so this time. A contrast-enhanced CT scan revealed a food bolus at the C6–C7 level, notably adjacent to an anterior C6–C7 osteophyte. After conservative measures proved ineffective, the food bolus was successfully removed via endoscopic removal.
Conclusion
This case highlights a rare but significant cause of esophageal food impaction: extrinsic structural compression by an anterior C6–C7 osteophyte. It underscores the importance of considering less common etiologies, particularly with recurrent impactions or when standard treatments fail. Advanced imaging, like CT scans, is crucial for identifying these atypical causes, guiding appropriate management, and ultimately improving patient outcomes.
Introduction
Esophageal food impaction is a common gastrointestinal issue that often presents in the emergency department. The incidence ranges from 13 to 25 cases per 100,000 people per year.1,2 Most cases present similarly: patients report dysphagia, odynophagia, globus sensation, regurgitation, and/or chest discomfort after ingesting meat.
These impactions are typically caused by underlying esophageal pathologies such as Schatzki’s ring, peptic strictures, or eosinophilic esophagitis. For individuals with such conditions, the recurrence rate of impaction is approximately 21%, and as high as 50% in those with eosinophilic esophagitis.2
Initial evaluation relies heavily on a thorough history and physical examination. Imaging is generally not required unless there is a concern for radiopaque foreign bodies (e.g., bones) or to assess for complications such as esophageal perforation. Incomplete obstructions may be managed conservatively. Interventions such as glucagon and carbonated beverages have shown limited benefit. However, if the impaction persists for more than 12–24 hours, or if there is complete obstruction leading to pooling of secretions or airway compromise, emergent endoscopy becomes necessary.3
While most esophageal food impactions stem from intrinsic esophageal abnormalities, rare cases may be due to extrinsic structural causes. This case report highlights one such instance.

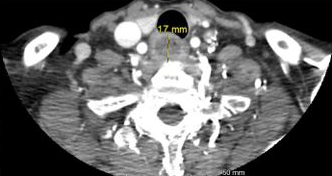
Figure 1. Sagittal and transverse views of esophageal food bolus impaction
Case
A 62-year-old female presented with a 12-hour history of food impaction following pork chop ingestion. She reported the sensation of food not passing completely into her stomach. She had experienced multiple similar episodes in the past but had always been able to regurgitate the bolus spontaneously. This time, repeated attempts to induce vomiting were unsuccessful. She had never previously required endoscopic intervention.
Her past medical history included atrial fibrillation (on rivaroxaban), chronic obstructive pulmonary disease (COPD), hypertension, hyperlipidemia, chronic neck and back pain managed with opioid-based analgesics, and tobacco use.
Upon arrival and throughout her stay in the emergency department, vital signs remained stable. Physical examination was largely unremarkable. There was no pooling of secretions, and the airway was patent and intact.
Laboratory tests—including complete blood count, basic metabolic panel, liver panel, and lipase—were within normal limits. A chest X-ray revealed no radiopaque foreign bodies. A contrast-enhanced computed tomography (CT) scan of the neck and chest identified a 3.0 × 1.2 × 1.7 cm food bolus (Figure 1) lodged at the C6–C7 level, adjacent to an anterior C6–C7 osteophyte (Figure 2).
While in the emergency department, the patient attempted to drink a carbonated beverage without relief. Glucagon was administered, but her symptoms persisted.
Gastroenterology was consulted, and the patient was admitted for emergent endoscopy. She was started on an intravenous proton pump inhibitor (PPI) and subsequently underwent esophagogastroduodenoscopy (EGD) with successful removal of the food bolus. She was discharged home on an oral PPI and referred for outpatient follow-up with gastroenterology for further evaluation.
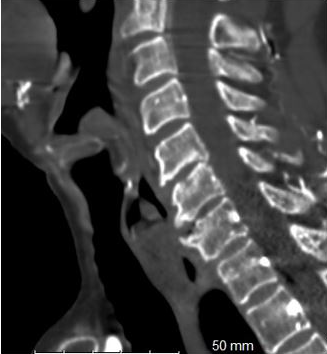
Figure 2. Sagittal views of C6-C7 anterior osteophyte.
Discussion
This case is particularly noteworthy and important because it highlights a rare cause of esophageal food impaction: an extrinsic structural compression from an anterior C6-C7 osteophyte. While most such impactions are attributed to intrinsic esophageal pathologies like Schatzki's ring or eosinophilic esophagitis, this case serves as a crucial reminder for clinicians to consider less common etiologies. The patient's history of recurring impactions, despite always self-resolving previously, underscores the need for thorough investigation when typical management fails. The use of a contrast-enhanced CT scan was instrumental in identifying the osteophyte, demonstrating the value of advanced imaging in atypical presentations. This case contributes significantly to the medical literature by broadening the differential diagnosis for esophageal food impaction. Recognizing such uncommon causes can prevent diagnostic delays and guide appropriate, individualized management, ultimately improving patient outcomes. It emphasizes that while conservative measures are often first-line, persistence of symptoms warrants a deeper look for underlying structural issues, even if they are extrinsic to the esophagus.
The World Society of Emergency Surgery (WSES) Guidelines estimate a false negative rate of up to 85% for esophageal food bolus impactions. Furthermore the WSES provides Grade 1B recommendations for CT imaging to be performed in patients with suspected perforation or other complications that may require interventional endoscopy, and states that CT is an essential tool in suspected ingestion of bone fragments with negative X-rays.4
According to Liu et al, CT demonstrated 100% sensitivity, 92.6% specificity, 100% negative predictive value and a 97.9% positive predictive value in assessing the presence of esophageal foreign bodies and suggested a reduction in complication rates and severity of complications prior to endoscopic evaluation.5 Additionally, Ma et al found statistical superiority of CT imaging versus plain radiographs in the diagnosis of patients found to have pointed or sharp thoracic esophageal foreign bodies.6
The current literature focuses on the ability of CT imaging to help establish the diagnosis of esophageal foreign bodies and reduce subsequent complications of a relatively frequent emergency department complaint. Not only did CT imaging help establish the diagnosis of an esophageal food impaction in our patient but also provided further information regarding the anatomical environment of the site where the patient had frequent and recurrent food impactions. Evaluation of the surrounding anatomy using CT imaging established a diagnosis of an anterior osteophyte at the level of the food impaction which gave further information for endoscopic and/or surgical planning prior to intervention.
References
- Gretarsdottir HM, Gunnarsdottir SA, Hardarson D, Jonsdottir HH. Etiology and management ofesophageal food impaction: A population-based study. Scand J Gastroenterol. 2015;50(9):1091–1098.
- Longstreth GF, Longstreth KJ, Yao JF. Esophageal food impaction: Epidemiology and therapy. Gastrointest Endosc. 2001;53(2):193–198.
- Tintinalli JE, Stapczynski JS, Ma OJ, Yealy DM, Meckler GD, Cline DM, eds. Tintinalli's Emergency Medicine: A Comprehensive Study Guide. 9th ed. McGraw Hill; 2020.
- Chirica M, Kelly MD, Siboni S, Aiolfi A, Riva CG, Asti E, Ferrari D, Leppäniemi A, Ten Broek RPG, Brichon PY, Kluger Y, Fraga GP, Frey G, Andreollo NA, Coccolini F, Frattini C, Moore EE, Chiara O, Di Saverio S, Sartelli M, Weber D, Ansaloni L, Biffl W, Corte H, Wani I, Baiocchi G, Cattan P, Catena F, Bonavina L. Esophageal emergencies: WSES guidelines. World J Emerg Surg. 2019 May 31;14:26.
- Liu YC, Zhou SH, Ling L. Value of helical computed tomography in the early diagnosis of esophageal foreign bodies in adults. Am J Emerg Med. 2013 Sep;31(9):1328-32. Epub 2013 Jul 27.
- Ma J, Kang DK, Bae JI, Park KJ, Sun JS. Value of MDCT in diagnosis and management of esophageal sharp or pointed foreign bodies according to level of esophagus. AJR Am J Roentgenol. 2013 Nov;201(5):W707-11.



